https://www.sciencedirect.com/science/article/pii/S000629522200106X
aDivisão de Endocrinologia, Departamento de Pediatria, Universidade da Califórnia, San Francisco, CA 94143, Estados Unidos;
bBrody School of Medicine, East Carolina University, Greenville, NC 27834, Estados Unidos;
cInstituto de Ciências da Saúde Ambiental e Departamento de Farmacologia, Wayne State University, Detroit, MI 48202, Estados Unidos;
dEscola de Ciências Ambientais e Biológicas, Rutgers University, New Brunswick, NJ 08901, Estados Unidos;
eUniversidade Sorbonne Paris Nord, Bobigny, INSERM U1124 (T3S), Paris, França;
fDepartamento de Bioquímica e Toxicologia, Universidade de Paris, INSERM U1224 (T3S), 75006 Paris, França;
gFaculdade de Saúde e Medicina, Universidade Nacional Australiana, Canberra, Austrália
hDivisão de Gastroenterologia, Hepatologia e Nutrição, Universidade de Louisville, Louisville, KY 40402, Estados Unidos;
Laboratório de Saúde e Doenças Ambientais, Universidade da Carolina do Sul, Columbia, SC 29208, Estados Unidos;
jFaculdade de Farmácia, Texas A&M University, College Station, TX 77843, Estados Unidos;
kGrupo de Pesquisa em Saúde Ocupacional e Ambiental, Universidade de Stirling, Stirling, Escócia, Reino Unido;
lUniv Rennes, INSERM, EHESP, IRSET – UMR_S 1085, 35000 Rennes, França;
mAmbiente Saudável e Estratégias de Disrupção Endócrina, Commonweal, Bolinas, CA 92924, Estados Unidos;
nDepartamento de Ciências Médicas, Universidade de Uppsala, Uppsala, Suécia;
oNorris Cotton Cancer Center, Departamento de Biologia Molecular e de Sistemas, Geisel School of Medicine em Dartmouth, Líbano, NH 03756, Estados Unidos;
pDepartamento de Citocinética, Instituto de Biofísica da Academia Tcheca de Ciências, Brno, República Tcheca.
Recebido em 8 de dezembro de 2021, revisado em 12 de março de 2022, aceito em 15 de março de 2022, disponível on-line em 5 de abril de 2022, versão do registro em 25 de abril de 2022 .
Destaques
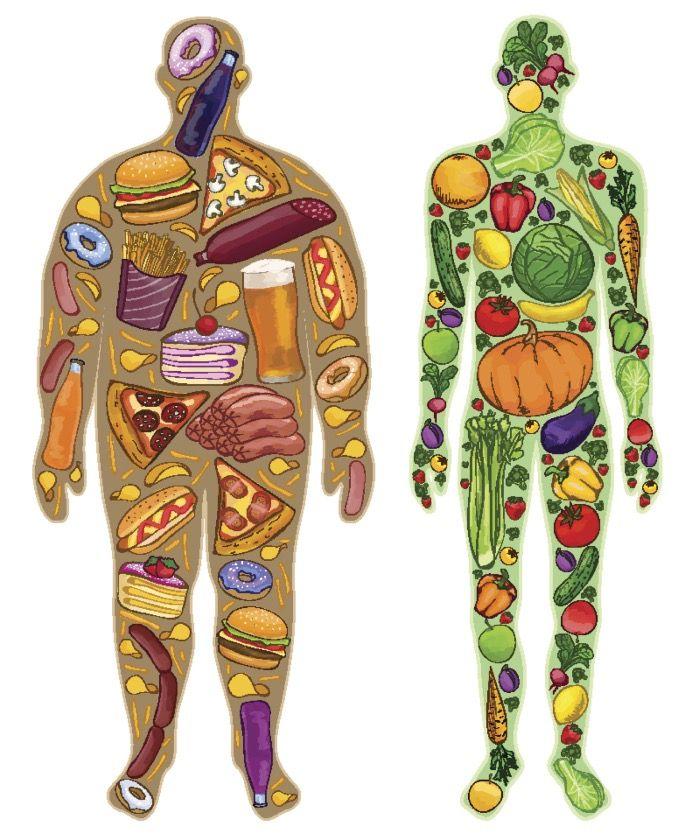
Há uma expansão global da obesidade e da pandemia de doenças não transmissíveis.
A obesidade é uma doença multifatorial, multiorgânica, multihormonal e multimecanística.
Influências genéticas e ambientais controlam a adiposidade e o ganho de peso.
Compreender os tecidos/órgãos, hormônios e mecanismos envolvidos na obesidade prepara o terreno para a compreensão das evidências da hipótese obesogênica.
Resumo
A obesidade é uma condição crônica e recorrente caracterizada pelo excesso de gordura corporal. Sua prevalência aumentou globalmente desde a década de 1970, e o número de pessoas obesas e com sobrepeso é agora maior do que aquelas com baixo peso. A obesidade é uma condição multifatorial e, como tal, muitos componentes contribuem para o seu desenvolvimento e patogênese. Esta é a primeira de três revisões complementares que consideram a obesidade (nt.: estão os fragmentos mais importantes dos textos das três, publicadas neste website. Os textos são longos e complexos, por isso escolhemos os aspectos que possam mais interessar a nós leigos, cidadãos e pais). Esta revisão se concentra na genética, vírus, resistência à insulina, inflamação, microbioma intestinal e ritmos circadianos que promovem a obesidade, juntamente com hormônios, fatores de crescimento e órgãos e tecidos que controlam seu desenvolvimento. Ele mostra que a regulação do balanço energético (ingestão versus gasto) depende da interação de uma variedade de hormônios do tecido adiposo, trato gastrointestinal, pâncreas, fígado e cérebro. Ela detalha como integrar neurotransmissores centrais e sinais metabólicos periféricos (por exemplo, leptina, insulina, grelina, peptídeo YY3-36) é essencial para controlar a homeostase energética e o comportamento alimentar. Descreve os diferentes tipos de adipócitos e como o desenvolvimento das células adiposas é controlado por hormônios e fatores de crescimento que atuam através de uma variedade de receptores, incluindo o receptor-gama ativado pelo proliferador de peroxissoma, retinóide X, insulina, estrogênio, andrógeno, glicocorticóide, hormônio da tireóide, fígado X, androstano constitutivo, pregnano X, farnesóide e receptores de hidrocarboneto aril. Finalmente, demonstra que a obesidade provavelmente tem origens no útero (nt.: aspecto importantíssimo porque estamos agredindo com as moléculas modernas sintéticas os que ainda nem nasceram. ESTAMOS DETERMINANDO A EXISTÊNCIA DESTA SÍNDROME NOS QUE PODERIAM NASCER SAUDÁVEIS). Compreender esses fatores bioquímicos de adiposidade e disfunção metabólica ao longo do ciclo de vida confere plausibilidade e credibilidade à “hipótese obesogênica” (ou seja, a importância de substâncias químicas ambientais que interrompem esses receptores para promover adiposidade ou alterar o metabolismo), elucidada mais detalhadamente na avaliações destas duas situações.
Resumo gráfico

1 . Introdução e tendências seculares
A obesidade é uma condição crônica e recidivante caracterizada pelo excesso de gordura corporal [1], [2]. Está entre os problemas de saúde globais mais críticos e uma pandemia crescente que afeta adultos, crianças e bebês [3], [4], [5]. As taxas de obesidade triplicaram desde a década de 1970, e a prevalência de obesidade em adultos nos EUA aumentou de 30,5% em 2000 para 42,4% em 2018, um aumento de 40% na frequência em menos de duas décadas [6]. Atualmente, existem mais indivíduos obesos globalmente do que aqueles que estão abaixo do peso [7], [8], [9]. (nt.: destaque dado pela tradução).
No entanto, esse aumento na prevalência da obesidade não se restringe aos humanos. Em 2011, Klimentidis e colegas [10] relataram pesos corporais médios na meia-idade de muitos animais, incluindo cães e gatos domésticos, primatas não humanos e roedores, independentemente das condições de vida (tanto selvagens quanto vivendo em colônias de pesquisa) também aumentou. Essas mudanças no peso dos animais em várias espécies sugerem que mudanças ambientais semelhantes impactaram tanto animais quanto humanos para promover a obesidade. Embora as mudanças no comportamento humano, sem dúvida, desempenhem um papel na manifestação da obesidade, mecanismos hormonais e bioquímicos específicos, fora de seu controle imediato, provavelmente contribuem.
Esta é a primeira de três revisões complementares com foco em obesidade e obesogênios. Esta primeira revisão delineia os órgãos e mecanismos responsáveis pela regulação do metabolismo e seu rígido controle por hormônios e seus respectivos receptores. A interrupção dessa regulação por hormônios ou outros estímulos ambientais pode levar à obesidade em qualquer momento do ciclo de vida, inclusive no pré-natal. A revisão complementar elucidará a química e a ação fisiopatológica dos obesogênicos – produtos químicos ambientais projetados para um propósito específico, como agrotóxicos, retardadores de chama ou plastificantes, mas que têm efeitos colaterais que interferem na ação hormonal – o que pode levar a alterações no metabolismo e, finalmente, à obesidade. A segunda revisão também estabelecerá o nexo causal entre os obesógenos e a obesidade, fornecendo explicitamente evidências que apoiam a “hipótese dos obesógenos” e discutirá as lacunas de pesquisa que devem ser exploradas. A terceira se concentrará em ensaios diretos e indiretos para detectar obesogênios.
2 . Obesidade e doença
[nota do website: não iremos transcrever todos os textos por serem técnicos e específicos, podendo tornar a leitura muito difícil e longa. Iremos somente colocar os aspectos que considerados relevantes para nós, os leigos.]
…………………………………………………………………………………………………..
3 . Desenvolvimento e função do tecido adiposo
…………………………………………………………………………………………………..
4 . Receptores envolvidos no controle do metabolismo energético
……………………………………………………………………………………………………
5 . Neuroendocrinologia da obesidade
……………………………………………………………………………………………………..
6 . Natureza heterogênea do controle de peso e adiposidade
……………………………………………………………………………………………………..
7 . Mecanismos fisiopatológicos que promovem obesidade
……………………………………………………………………………………………………..
8 . Origens fetais da obesidade
……………………………………………………………………………………………………..
9 . Conclusões
Esta revisão concentrou-se nos tecidos/órgãos, hormônios, vias e mecanismos que desempenham papéis-chave no metabolismo para induzir o tecido adiposo, resultando em obesidade. A obesidade é uma doença multifuncional, multi-tecidos, multi-hormônio, multirreceptor e multimecanismo. Quando a obesidade resulta do aumento do VAT ou da gordura do fígado com grandes células de gordura, inflamação e resistência à insulina e à leptina, também está associada a vários distúrbios metabólicos, incluindo DM2 (nt.: diabetes tipo 2), DHGNA (nt.: doença hepática gordurosa não alcoólica), DCV (nt.: doença cardiovascular) e alguns tipos de câncer. Por outro lado, quando a obesidade resulta do aumento da TAS com pequenos adipócitos, inflamação limitada e atividade normal de insulina e leptina, há, em alguns casos, falta de perturbação metabólica correspondente, pelo menos inicialmente. A natureza multifuncional da obesidade resulta de muitos fatores de interação altamente coordenados que desempenham um papel na obesidade, incluindo fatores genéticos e ambientais. O ambiente inclui nutrição, exercício, vírus, microbioma, ritmos circadianos (esta revisão) e produtos químicos ambientais (discutidos na revisão complementar). Os fatores ambientais atuam nos complexos sistemas de órgãos interativos que controlam o metabolismo, incluindo tecido adiposo, trato gastrointestinal, músculo, pâncreas, fígado e várias partes do cérebro, que integram o controle do comportamento alimentar, incluindo a alimentação hedônica homeostática. O controle do desenvolvimento do tecido adiposo, bem como o número e tamanho dos adipócitos, depende da atividade e interação de uma variedade de fatores de transcrição, incluindo os dois reguladores mestres da adipogênese: PPARγ; e RXR , que pode ativar a adipogênese sozinho ou como um heterodímero com PPARγ. Os hormônios insulina, estrogênio, andrógeno, glicocorticóide e hormônio tireoidiano também desempenham papéis importantes no metabolismo e na adipogênese, ligando-se aos seus receptores. Outros fatores de transcrição do fígado modulam sinais metabólicos específicos, que podem levar à doença quando disfuncionais. O LXR, embora não seja ativado por hormônios específicos, regula a diferenciação dos adipócitos, o transporte de colesterol e o acúmulo de triglicerídeos. O PXR e o CAR parecem atuar em conjunto com o PPARγ e regulam a homeostase da glicose e energia e o metabolismo imunológico e lipídico. O FXR regula a síntese de ácidos biliares e o metabolismo lipídico, e o AhR pode resultar em resistência à insulina hepática. A ativação desses receptores pode resultar em hiperinsulinemia, resistência à leptina e ganho de peso.
Os tecidos e órgãos que controlam o metabolismo e, portanto, o ganho de peso, se comunicam por meio de uma rede de hormônios e neurotransmissores. Por exemplo, leptina, resistina e adiponectina são induzidas a partir de adipócitos; grelina e GIP do estômago; CCK, GLP-1, OXM e PYY 3-36 do trato gastrointestinal; insulina e glucagon do pâncreas; NPY-AgRP e POMC de neurônios hipotalâmicos; dopamina do VTA e NA; bem como estrogênio, andrógeno, hormônio tireoidiano e cortisol de suas respectivas glândulas endócrinas.
Embora a obesidade possa ocorrer ao longo da vida, ela pode ter suas origens durante o desenvolvimento fetal e a infância e, portanto, é regulada por mudanças na regulação epigenética ou na programação de desenvolvimento da expressão gênica. Essas perturbações são particularmente suscetíveis a influências ambientais.
Esta revisão do metabolismo destaca os órgãos e mecanismos responsáveis pela regulação da adiposidade. Também estabelece a hipótese de que substâncias químicas ambientais capazes de interromper esses mecanismos, denominadas obesogênicos, podem levar à obesidade. Numerosos compostos, alguns nutricionais e alguns disruptores endócrinos (EDCs/endocrine disruptors chemicals), podem afetar o controle hormonal da diferenciação, desenvolvimento, crescimento e/ou manutenção do tecido adiposo. Essas alterações subsequentemente resultam em efeitos diferenciais nos depósitos de gordura que podem afetar a disfunção metabólica. Assim, propomos que a mudança na prevalência e gravidade da obesidade é, pelo menos em parte, devido à ocorrência e acúmulo de várias alterações ambientais – na forma de má nutrição ou EDCs obesogênicos – em uma população geneticamente suscetível, o mais suscetível é o feto. O segundo artigo complementar revisará a plausibilidade, mecanismo e evidência para esses obesogênicos –in vitro , animais e humanos.
Financiamento
Christopher Kassotis, NIH, R00ES030405.
Dominique Lagadic-Gossman, European Union Horizon 2020 Research and Innovation Program, Oberon #825712.
Vesna Munic Kos, Swedish Research Council for Sustainable Development (FORMAS) #2019-00375.
Troy Roepke, NIH, R01MH12 3544, P30ES005022, USDA/NIFA NJ6195.
Jan Vondracek, Czech Science Foundation #21-005335, Institute of Biophysics of the Czech Academy of Science, RVO-68081707.
Robert Barouki, European Union Horizon 2020 Research and Innovation Program, Oberon #825712.
Amita Bansal, Diabetes Australia #S5610040.
Mathew Cave, NIH, R35ES028373, R01ES032189, T32ES011564, P42ES023716, P30ES030283, R21ES031510.
Saurabh Chatterjee, NIH, P20GM103641, P01ES028942, P01AT003961, DoD-IIRFA W81XWH1810374.
Mahua Choudhury, Morris L Lichtenstein Jr Medical Research Foundation.
David Collier, NIH, P30ES025128.
Referências
[1] A.M. Jastreboff, C.M. Kotz, S. Kahan, A.S. Kelly, S.B. Heymsfield Obesity as a disease: the obesity society 2018 position statement Obesity (Silver Spring), 27 (1) (2019), pp. 7-9 View PDF CrossRefView Record in ScopusGoogle Scholar
[2] J.I. Mechanick, A.J. Garber, Y. Handelsman, W.T. Garvey American association of clinical endocrinologists’ position statement on obesity and obesity medicine Endocr Pract, 18 (5) (2012), pp. 642-648 ArticleDownload PDFView Record in ScopusGoogle Scholar
[3]L.M. Jaacks, S. Vandevijvere, A. Pan, C.J. McGowan, C. Wallace, F. Imamura, D. Mozaffarian, B. Swinburn, M. Ezzati The obesity transition: stages of the global epidemic Lancet. Diabet. Endocrinol., 7 (3) (2019), pp. 231-240 ArticleDownload PDFView Record in ScopusGoogle Scholar
[4] M. Blüher Obesity: global epidemiology and pathogenesis Nat. Rev. Endocrinol., 15 (5) (2019), pp. 288-298 View PDF CrossRefView Record in ScopusGoogle Scholar
[5] W.J. Morales Camacho, J.M. Molina Díaz, S. Plata Ortiz, J.E. Plata Ortiz, M.A. Morales Camacho, B.P. Calderón Childhood obesity: aetiology, comorbidities, and treatment Diabetes Metab. Res. Rev., 35 (8) (2019), Article e3203 View Record in ScopusGoogle Scholar
[6] C.M. Hales, M.D. Carroll, C.D. Fryar, C.L. Ogden, Prevalence of Obesity Among Adults and Youth: United States, 2015-2016, NCHS data brief (288) (2017) 1-8. Google Scholar
[7] E.P. Williams, M. Mesidor, K. Winters, P.M. Dubbert, S.B. Wyatt Overweight and obesity: prevalence, consequences, and causes of a growing public health problem Curr. Obesity Rep., 4 (3) (2015), pp. 363-370 View PDF CrossRefView Record in ScopusGoogle Scholar
[8] M. Ng, T. Fleming, M. Robinson, B. Thomson, N. Graetz, C. Margono, E.C. Mullany, S. Biryukov, C. Abbafati, S.F. Abera, J.P. Abraham, N.M. Abu-Rmeileh, T. Achoki, F.S. AlBuhairan, Z.A. Alemu, R. Alfonso, M.K. Ali, R. Ali, N.A. Guzman, W. Ammar, P. Anwari, A. Banerjee, S. Barquera, S. Basu, D.A. Bennett, Z. Bhutta, J. Blore, N. Cabral, I.C. Nonato, J.C. Chang, R. Chowdhury, K.J. Courville, M.H. Criqui, D.K. Cundiff, K.C. Dabhadkar, L. Dandona, A. Davis, A. Dayama, S.D. Dharmaratne, E.L. Ding, A.M. Durrani, A. Esteghamati, F. Farzadfar, D.F. Fay, V.L. Feigin, A. Flaxman, M.H. Forouzanfar, A. Goto, M.A. Green, R. Gupta, N. Hafezi-Nejad, G.J. Hankey, H.C. Harewood, R. Havmoeller, S. Hay, L. Hernandez, A. Husseini, B.T. Idrisov, N. Ikeda, F. Islami, E. Jahangir, S.K. Jassal, S.H. Jee, M. Jeffreys, J.B. Jonas, E.K. Kabagambe, S.E. Khalifa, A.P. Kengne, Y.S. Khader, Y.H. Khang, D. Kim, R.W. Kimokoti, J.M. Kinge, Y. Kokubo, S. Kosen, G. Kwan, T. Lai, M. Leinsalu, Y. Li, X. Liang, S. Liu, G. Logroscino, P.A. Lotufo, Y. Lu, J. Ma, N.K. Mainoo, G.A. Mensah, T.R. Merriman, A.H. Mokdad, J. Moschandreas, M. Naghavi, A. Naheed, D. Nand, K.M. Narayan, E.L. Nelson, M.L. Neuhouser, M.I. Nisar, T. Ohkubo, S.O. Oti, A. Pedroza, D. Prabhakaran, N. Roy, U. Sampson, H. Seo, S.G. Sepanlou, K. Shibuya, R. Shiri, I. Shiue, G.M. Singh, J.A. Singh, V. Skirbekk, N.J. Stapelberg, L. Sturua, B.L. Sykes, M. Tobias, B.X. Tran, L. Trasande, H. Toyoshima, S. van de Vijver, T.J. Vasankari, J.L. Veerman, G. Velasquez-Melendez, V.V. Vlassov, S.E. Vollset, T. Vos, C. Wang, X. Wang, E. Weiderpass, A. Werdecker, J.L. Wright, Y.C. Yang, H. Yatsuya, J. Yoon, S.J. Yoon, Y. Zhao, M. Zhou, S. Zhu, A.D. Lopez, C.J. Murray, E. Gakidou Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013 Lancet, 384 (9945) (2014), pp. 766-781 ArticleDownload PDFGoogle Scholar
[9] C.L. Ogden, M.D. Carroll, C.D. Fryar, K.M. Flegal, Prevalence of Obesity Among Adults and Youth: United States, 2011-2014, NCHS data brief (219) (2015) 1-8. Google Scholar
[10] Y.C. Klimentidis, T.M. Beasley, H.Y. Lin, G. Murati, G.E. Glass, M. Guyton, W. Newton, M. Jorgensen, S.B. Heymsfield, J. Kemnitz, L. Fairbanks, D.B. Allison Canaries in the coal mine: a cross-species analysis of the plurality of obesity epidemics Proc. Biol. Sci., 278 (1712) (2011), pp. 1626-1632 View PDF CrossRefView Record in ScopusGoogle Scholar
[11] L. Landsberg, L.J. Aronne, L.J. Beilin, V. Burke, L.I. Igel, D. Lloyd-Jones, J. Sowers Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment: a position paper of the obesity society and the American society of hypertension J. Clin. Hypertens. (Greenwich), 15 (1) (2013), pp. 14-33 View PDF CrossRefView Record in ScopusGoogle Scholar
[12] C. Andolfi, P.M. Fisichella Epidemiology of obesity and associated comorbidities J. Laparoendosc Adv. Surg. Tech. A, 28 (8) (2018), pp. 919-924 View Record in ScopusGoogle Scholar
[13] N. Stefan Causes, consequences, and treatment of metabolically unhealthy fat distribution, The Lancet Diabet. Endocrinol., 8 (7) (2020), pp. 616-627 ArticleDownload PDFView Record in ScopusGoogle Scholar
[14] J.C. Chan, J.C. Cheung, C.D. Stehouwer, J.J. Emeis, P.C. Tong, G.T. Ko, J.S. Yudkin The central roles of obesity-associated dyslipidaemia, endothelial activation and cytokines in the Metabolic Syndrome–an analysis by structural equation modelling Int. J. Obesity Related Metabol. Disorders: J. Int. Assoc. Study Obesity, 26 (7) (2002), pp. 994-1008 View PDF CrossRefView Record in ScopusGoogle Scholar
[15] A.K. Loomis, S. Kabadi, D. Preiss, C. Hyde, V. Bonato, M. St Louis, J. Desai, J.M. Gill, P. Welsh, D. Waterworth, N. Sattar Body mass index and risk of nonalcoholic fatty liver disease: two electronic health record prospective studies J. Clin. Endocrinol. Metabol., 101 (3) (2016), pp. 945-952 View PDF CrossRefGoogle Scholar
[16] P. Mathieu, I. Lemieux, J.P. Després Obesity, inflammation, and cardiovascular risk Clin. Pharmacol. Ther., 87 (4) (2010), pp. 407-416 View PDF CrossRefView Record in ScopusGoogle Scholar
[nota do website: como são muitas as referência e no momento da transcrição, ocorre esse descompasso com a configuração, deixaremos de fazer as adequações das restantes 391 citações pelo trabalho desnecessário para o conhecimento destas informações. Estão todas abaixo, mas com uma configuração inadequada, mas presente.]
S.S. Virani, A. Alonso, H.J. Aparicio, E.J. Benjamin, M.S. Bittencourt, C.W. Callaway, A.P. Carson, A.M. Chamberlain, S. Cheng, F.N. Delling, M.S.V. Elkind, K.R. Evenson, J.F. Ferguson, D.K. Gupta, S.S. Khan, B.M. Kissela, K.L. Knutson, C.D. Lee, T.T. Lewis, J. Liu, M.S. Loop, P.L. Lutsey, J. Ma, J. Mackey, S.S. Martin, D.B. Matchar, M.E. Mussolino, S.D. Navaneethan, A.M. Perak, G.A. Roth, Z. Samad, G.M. Satou, E.B. Schroeder, S.H. Shah, C.M. Shay, A. Stokes, L.B. VanWagner, N.Y. Wang, C.W. Tsao
Heart disease and stroke statistics-2021 Update: a report from the american heart association
Circulation, 143 (8) (2021), pp. e254-e743
S.M. Koroukian, W. Dong, N.A. Berger
Changes in age distribution of obesity-associated cancers
JAMA Network Open, 2 (8) (2019), Article e199261 View PDF
CrossRefView Record in ScopusGoogle Scholar[19]
B.C.M. Stephan, R. Birdi, E.Y.H. Tang, T.D. Cosco, L.M. Donini, S. Licher, M.A. Ikram, M. Siervo, L. Robinson
Secular trends in dementia prevalence and incidence worldwide: a systematic review
J. Alzheimers Dis, 66 (2) (2018), pp. 653-680 View PDF
CrossRefView Record in ScopusGoogle Scholar[20]
C.P. Benziger, G.A. Roth, A.E. Moran
The global burden of disease study and the preventable burden of NCD
Glob Heart, 11 (4) (2016), pp. 393-397
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[21]Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016, Lancet 390(10100) (2017) 1151-1210.
J. Bhattacharya, M.K. Bundorf
The incidence of the healthcare costs of obesity
J. Health Econ., 28 (3) (2009), pp. 649-658
ArticleDownload PDFView Record in ScopusGoogle Scholar[23]
S.A. Xanthakos, J.E. Lavine, K.P. Yates, J.B. Schwimmer, J.P. Molleston, P. Rosenthal, K.F. Murray, M.B. Vos, A.K. Jain, A.O. Scheimann, T. Miloh, M. Fishbein, C.A. Behling, E.M. Brunt, A.J. Sanyal, J. Tonascia
Progression of fatty liver disease in children receiving standard of care lifestyle advice
Gastroenterology, 159 (5) (2020), pp. 1731-1751.e10
ArticleDownload PDFView Record in ScopusGoogle Scholar[24]
P. Bjornstad, K.L. Drews, S. Caprio, R. Gubitosi-Klug, D.M. Nathan, B. Tesfaldet, J. Tryggestad, N.H. White, P. Zeitler
Long-term complications in youth-onset type 2 diabetes
New Engl. J. Med., 385 (5) (2021), pp. 416-426
View Record in ScopusGoogle Scholar[25]
J.M. Lawrence, J. Divers, S. Isom, S. Saydah, G. Imperatore, C. Pihoker, S.M. Marcovina, E.J. Mayer-Davis, R.F. Hamman, L. Dolan, D. Dabelea, D.J. Pettitt, A.D. Liese
Trends in prevalence of Type 1 and Type 2 diabetes in children and adolescents in the US, 2001–2017
JAMA, 326 (8) (2021), pp. 717-727 View PDF
CrossRefView Record in ScopusGoogle Scholar[26]
J. Dobner, S. Kaser
Body mass index and the risk of infection – from underweight to obesity
Clin. Microbiol. Infect., 24 (1) (2018), pp. 24-28
ArticleDownload PDFView Record in ScopusGoogle Scholar[27]
E. Korakas, I. Ikonomidis, F. Kousathana, K. Balampanis, A. Kountouri, A. Raptis, L. Palaiodimou, A. Kokkinos, V. Lambadiari
Obesity and COVID-19: immune and metabolic derangement as a possible link to adverse clinical outcomes
Am. J. Physiol. Endocrinol. Metabol., 319 (1) (2020), pp. E105-E109 View PDF
CrossRefView Record in ScopusGoogle Scholar[28]
B.M. Popkin, S. Du, W.D. Green, M.A. Beck, T. Algaith, C.H. Herbst, R.F. Alsukait, M. Alluhidan, N. Alazemi, M. Shekar
Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships
Obes Rev, 21 (11) (2020), Article e13128
View Record in ScopusGoogle Scholar[29]
J.M. Chan, E.B. Rimm, G.A. Colditz, M.J. Stampfer, W.C. Willett
Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men
Diabetes Care, 17 (1994), pp. 961-969 View PDF
CrossRefView Record in ScopusGoogle Scholar[30]
T. McLaughlin, F. Abbasi, K. Cheal, J. Chu, C. Lamendola, G.M. Reaven
Use of metabolic markers to identify overweight individuals who are insulin resistant
Ann. Int. Med., 139 (2003), pp. 802-809 View PDF
CrossRefView Record in ScopusGoogle Scholar[31]
D.L. Chen, C. Liess, A. Poljak, A. Xu, J. Zhang, C. Thoma, M. Trenell, B. Milner, A.B. Jenkins, D.J. Chisholm, D. Samocha-Bonet, J.R. Greenfield
Phenotypic characterization of insulin-resistant and insulin-sensitive obesity
J. Clin. Endocrinol. Metab., 100 (11) (2015), pp. 4082-4091 View PDF
CrossRefView Record in ScopusGoogle Scholar[32]D. Samocha-Bonet, V.D. Dixit, C.R. Kahn, R.L. Leibel, X. Lin, M. Nieuwdorp, K.H. Pietiläinen, R. Rabasa-Lhoret, M. Roden, P.E. Scherer, e. al., Metabolically healthy and unhealthy obese–the 2013 Stock Conference report, Obes. Rev. 15 (2014) 697-708.
G.I. Smith, B. Mittendorfer, S. Klein
Metabolically healthy obesity: facts and fantasies
J. Clin. Invest, 129 (10) (2019), pp. 3978-3989 View PDF
CrossRefView Record in ScopusGoogle Scholar[34]
M. Blüher
Metabolically healthy obesity
Endocr. Rev., 41 (3) (2020), pp. 405-420
View Record in ScopusGoogle Scholar[35]
Z. Zhou, J. Macpherson, S.R. Gray, J.M.R. Gill, P. Welsh, C. Celis-Morales, N. Sattar, J.P. Pell, F.K. Ho
Are people with metabolically healthy obesity really healthy? A prospective cohort study of 381,363 UK Biobank participants
Diabetologia, 64 (9) (2021), pp. 1963-1972 View PDF
CrossRefView Record in ScopusGoogle Scholar[36]
F. Abbasi, J.W. Chu, C. Lamendola, T. McLaughlin, J. Hayden, G.M. Reaven, P.D. Reaven
Discrimination between obesity and insulin resistance in the relationship with adiponectin
Diabetes, 53 (3) (2004), pp. 585-590 View PDF
CrossRefView Record in ScopusGoogle Scholar[37]
C. Voulgari, N. Tentolouris, P. Dilaveris, D. Tousoulis, N. Katsilambros, C. Stefanadis
Increased heart failure risk in normal-weight people with metabolic syndrome compared with metabolically healthy obese individuals
J. Am. Coll. Cardiol., 58 (13) (2011), pp. 1343-1350
ArticleDownload PDFView Record in ScopusGoogle Scholar[38]
J. Araújo, J. Cai, J. Stevens
Prevalence of optimal metabolic health in American adults: national health and nutrition examination survey 2009–2016
Metab. Syndr. Relat. Disord., 17 (1) (2019), pp. 46-52 View PDF
CrossRefView Record in ScopusGoogle Scholar[39]
E.L. Thomas, J.A. Fitzpatrick, S.J. Malik, S.D. Taylor-Robinson, J.D. Bell
Whole body fat: content and distribution
Prog. Nucl. Magn. Reson. Spectrosc., 73 (2013), pp. 56-80
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[40]
A.L. Rosenbloom, J. Guevara Aguirre, R.G. Rosenfeld, P.J. Fielder
The little women of Loja–growth hormone-receptor deficiency in an inbred population of southern Ecuador
N Engl J Med., 323 (20) (1990), pp. 1367-1374
View Record in ScopusGoogle Scholar[41]
F.F. Chehab
Obesity and lipodystrophy–where do the circles intersect?
Endocrinology, 149 (3) (2008), pp. 925-934 View PDF
CrossRefView Record in ScopusGoogle Scholar[42]
M.W. Schwartz, R.J. Seeley, L.M. Zeltser, A. Drewnowski, E. Ravussin, L.M. Redman, R.L. Leibel
Obesity pathogenesis: an endocrine society scientific statement
Endocr. Rev., 38 (4) (2017), pp. 267-296 View PDF
CrossRefView Record in ScopusGoogle Scholar[43]
S. Basu, P. Yoffe, N. Hills, R.H. Lustig
The relationship of sugar to population-level diabetes prevalence: an econometric analysis of repeated cross-sectional data
PLoS ONE, 8 (2) (2013), Article e57873 View PDF
CrossRefView Record in ScopusGoogle Scholar[44]
J. Sepúlveda, C. Murray
The state of global health in 2014
Science, 345 (6202) (2014), pp. 1275-1278 View PDF
CrossRefView Record in ScopusGoogle Scholar[45]
Y.W. Park, S. Zhu, L. Palaniappan, S. Heshka, M.R. Carnethon, S.B. Heymsfield
The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994
Arch. Intern. Med., 163 (4) (2003), pp. 427-436
View Record in ScopusGoogle Scholar[46]
E.J. Gallagher, D. LeRoith
Obesity and diabetes: the increased risk of cancer and cancer-related mortality
Physiol. Rev., 95 (3) (2015), pp. 727-748 View PDF
CrossRefView Record in ScopusGoogle Scholar[47]
E.E. Calle, M.J. Thun, J.M. Petrelli, C. Rodriguez, C.W. Heath Jr.
Body-mass index and mortality in a prospective cohort of U.S. adults
New Engl. J. Med., 341 (15) (1999), pp. 1097-1105
R.P. Wildman, P. Muntner, K. Reynolds, A.P. McGinn, S. Rajpathak, J. Wylie-Rosett, M.R. Sowers
The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004)
Arch. Intern. Med., 168 (15) (2008), pp. 1617-1624 View PDF
CrossRefView Record in ScopusGoogle Scholar[49]
P. Dempster, S. Aitkens
A new air displacement method for the determination of human body composition
Med. Sci. Sports Exerc., 27 (12) (1995), pp. 1692-1697
View Record in ScopusGoogle Scholar[50]
M.M. Ibrahim
Subcutaneous and visceral adipose tissue: structural and functional differences
Obes. Rev., 11 (1) (2010), pp. 11-18
View Record in ScopusGoogle Scholar[51]
R. Ter Horst, I.C.L. van den Munckhof, K. Schraa, R. Aguirre-Gamboa, M. Jaeger, S.P. Smeekens, T. Brand, H. Lemmers, H. Dijkstra, T.E. Galesloot, J. de Graaf, R.J. Xavier, Y. Li, L.A.B. Joosten, J.H.W. Rutten, M.G. Netea, N.P. Riksen
Sex-specific regulation of inflammation and metabolic syndrome in obesity
Arterioscler Thromb. Vasc. Biol., 40 (7) (2020), pp. 1787-1800 View PDF
CrossRefView Record in ScopusGoogle Scholar[52]
Y.S. Torre, R. Wadeea, V. Rosas, K.L. Herbst
Lipedema: friend and foe
Hormone Mol. Biol. Clin. Investigat., 33 (1) (2018)
S.A. Porter, J.M. Massaro, U. Hoffmann, R.S. Vasan, C.J. O’Donnel, C.S. Fox
Abdominal subcutaneous adipose tissue: a protective fat depot?
Diabetes Care, 32 (6) (2009), pp. 1068-1075 View PDF
CrossRefView Record in ScopusGoogle Scholar[54]
B.S. Mohammed, S. Cohen, D. Reeds, V.L. Young, S. Klein
Long-term effects of large-volume liposuction on metabolic risk factors for coronary heart disease
Obesity (Silver Spring), 16 (12) (2008), pp. 2648-2651 View PDF
CrossRefView Record in ScopusGoogle Scholar[55]
M. Bastien, P. Poirier, P. Brassard, B.J. Arsenault, O.F. Bertrand, J.P. Després, O. Costerousse, M.E. Piché
Effect of PPARγ agonist on aerobic exercise capacity in relation to body fat distribution in men with type 2 diabetes mellitus and coronary artery disease: a 1-yr randomized study
Am. J. Physiol. Endocrinol. Metabol., 317 (1) (2019), pp. E65-E73 View PDF
CrossRefView Record in ScopusGoogle Scholar[56]
M. Kabir, K.J. Catalano, S. Ananthnarayan, S.P. Kim, G.W. Van Citters, M.K. Dea, R.N. Bergman
Molecular evidence supporting the portal theory: a causative link between visceral adiposity and hepatic insulin resistance
Am. J. Physiol. Endocrinol. Metab., 288 (2) (2004), pp. E454-E461
O.V. Gruzdeva, A.D. Borodkina, O.E. Akbasheva, Y.A. Dileva, L.V. Antonova, V.G. Matveeva, E.G. Uchasova, S.V. Ivanov, E.V. Belik, E.V. Fanaskova, V.N. Karetnikova, A.N. Kokov, O.L. Barbarash
Influence of visceral obesity on the secretion of adipokines with epicardial adipocytes in patients with coronary heart disease
Ter Arkh, 90 (10) (2018), pp. 71-78
View Record in ScopusGoogle Scholar[58]
P. Björntorp
How should obesity be defined?
J. Int. Med., 227 (3) (1990), pp. 147-149 View PDF
CrossRefView Record in ScopusGoogle Scholar[59]
E. Ravussin, S.R. Smith
Increased fat intake, impaired fat oxidation, and failure of fat cell proliferation result in ectopic fat storage, insulin resistance, and type 2 diabetes mellitus
Ann. NY Acad. Sci., 967 (2002), pp. 363-378
View Record in ScopusGoogle Scholar[60]
E. D’Adamo, A.M. Cali, R. Weiss, N. Santoro, B. Pierpont, V. Northrup, S. Caprio
Central role of fatty liver in the pathogenesis of insulin resistance in obese adolescents
Diabetes Care, 33 (8) (2010), pp. 1817-1822 View PDF
CrossRefView Record in ScopusGoogle Scholar[61]
K.A. Britton, C.S. Fox
Ectopic fat depots and cardiovascular disease
Circulation, 124 (24) (2011), pp. e837-e841 View PDF
CrossRefView Record in ScopusGoogle Scholar[62]
R.H. Lustig, K. Mulligan, S.M. Noworolski, A. Gugliucci, A. Erkin-Cakmak, M.J. Wen, V.W. Tai, J.M. Schwarz
Isocaloric fructose restriction and metabolic improvement in children with obesity and metabolic syndrome
Obesity (Silver Spring), 24 (2016), pp. 453-460 View PDF
CrossRefView Record in ScopusGoogle Scholar[63]J.M. Schwarz, S.M. Noworolski, A. Erkin-Cakmak, K. N.J., M.J. Wen, V.W. Tai, G.M. Jones, S.P. Palii, M. Velasco-Alin, K. Pan, B.W. Patterson, A. Gugliucci, R.H. Lustig, K. Mulligan, Impact of dietary fructose restriction on liver fat, de novo lipogenesis, and insulin kinetics in children with obesity, Gastroenterology 153 (2017) 743-752.
E.H. Lee, J.Y. Kim, H.R. Yang
Association between ectopic pancreatic and hepatic fat and metabolic risk factors in children with non-alcoholic fatty liver disease
Pediatric Obesity, 16 (10) (2021), Article e12793
View Record in ScopusGoogle Scholar[65]
J.A. Isserow, E.S. Siegelman, J. Mammone
Focal fatty infiltration of the pancreas: MR characterization with chemical shift imaging
Am. J. Roentgenol., 173 (5) (1999), pp. 1263-1265 View PDF
CrossRefView Record in ScopusGoogle Scholar[66]
E. Blaak
Gender differences in fat metabolism
Curr. Opin. Clin. Nutrit. Metabol. Care, 4 (6) (2001), pp. 499-502
View Record in ScopusGoogle Scholar[67]
W.B. Kannel, M.C. Hjortland, P.M. McNamara, T. Gordon
Menopause and risk of cardiovascular disease: the Framingham study
Ann. Int. Med., 85 (4) (1976), pp. 447-452 View PDF
CrossRefView Record in ScopusGoogle Scholar[68]
C.A. Derby, S.L. Crawford, R.C. Pasternak, M. Sowers, B. Sternfeld, K.A. Matthews
Lipid changes during the menopause transition in relation to age and weight: the Study of Women’s Health Across the Nation
Am. J. Epidemiol., 169 (11) (2009), pp. 1352-1361 View PDF
CrossRefView Record in ScopusGoogle Scholar[69]
S. Qian, Y. Tang, Q.-Q. Tang
Adipose tissue plasticity and the pleiotropic roles of BMP signaling
J. Biol. Chem., 296 (2021), p. 100678
ArticleDownload PDFView Record in ScopusGoogle Scholar[70]
U. Smith, B.B. Kahn
Adipose tissue regulates insulin sensitivity: role of adipogenesis, de novo lipogenesis and novel lipids
J. Int. Med., 280 (5) (2016), pp. 465-475 View PDF
CrossRefView Record in ScopusGoogle Scholar[71]
P. Arner
Fat tissue growth and development in humans
Nestle Nutrition Institute Workshop Series, 89 (2018), pp. 37-45 View PDF
CrossRefView Record in ScopusGoogle Scholar[72]
K.L. Spalding, E. Arner, P.O. Westermark, S. Bernard, B.A. Buchholz, O. Bergmann, L. Blomqvist, J. Hoffstedt, E. Naslund, T. Britton, H. Concha, M. Hassan, M. Ryden, J. Frisen, P. Arner
Dynamics of fat cell turnover in humans
Nature, 453 (7196) (2008), pp. 783-787 View PDF
CrossRefView Record in ScopusGoogle Scholar[73]
B.J. Feldman, R.S. Streeper, R.V. Farese Jr., K.R. Yamamoto
Myostatin modulates adipogenesis to generate adipocytes with favorable metabolic effects
PNAS, 103 (42) (2006), pp. 15675-15680 View PDF
CrossRefView Record in ScopusGoogle Scholar[74]
M.D. Lynes, Y.-H. Tseng
Deciphering adipose tissue heterogeneity
Ann. N. Y. Acad. Sci., 1411 (1) (2018), pp. 5-20 View PDF
CrossRefView Record in ScopusGoogle Scholar[75]
S. Ussar, K.Y. Lee, S.N. Dankel, J. Boucher, M.F. Haering, A. Kleinridders, T. Thomou, R. Xue, Y. Macotela, A.M. Cypess, Y.H. Tseng, G. Mellgren, C.R. Kahn
ASC-1, PAT2, and P2RX5 are cell surface markers for white, beige, and brown adipocytes
Sci. Transl. Med., 6 (247) (2014), p. 247ra103
View Record in ScopusGoogle Scholar[76]S. Cinti, Pink Adipocytes, Trends in endocrinology and metabolism: TEM 29(9) (2018) 651-666.
J.-B. Funcke, P.E. Scherer
Beyond adiponectin and leptin: adipose tissue-derived mediators of inter-organ communication
J. Lipid Res., 60 (10) (2019), pp. 1648-1684 View PDF
S. Heinonen, R. Jokinen, A. Rissanen, K.H. Pietiläinen
White adipose tissue mitochondrial metabolism in health and in obesity
Obes. Rev., 21 (2) (2020), Article e12958
View Record in ScopusGoogle Scholar[79]
L. Vishvanath, R.K. Gupta
Contribution of adipogenesis to healthy adipose tissue expansion in obesity
J. Clin. Invest., 129 (10) (2019), pp. 4022-4031 View PDF
CrossRefView Record in ScopusGoogle Scholar[80]G.H. Goossens, The Metabolic Phenotype in Obesity: Fat Mass, Body Fat Distribution, and Adipose Tissue Function, Obesity facts 10(3) (2017) 207-215.
A.C. Carpentier, D.P. Blondin, K.A. Virtanen, D. Richard, F. Haman, É.E. Turcotte
Brown adipose tissue energy metabolism in humans
Front. Endocrinol., 9 (2018), p. 447
View Record in ScopusGoogle Scholar[82]
A.M. Cypess, Y.-C. Chen, C. Sze, K. Wang, J. English, O. Chan, A.R. Holman, I. Tal, M.R. Palmer, G.M. Kolodny, C.R. Kahn
Cold but not sympathomimetics activates human brown adipose tissue in vivo
PNAS, 109 (25) (2012), pp. 10001-10005 View PDF
CrossRefView Record in ScopusGoogle Scholar[83]
L. Sidossis, S. Kajimura
Brown and beige fat in humans: thermogenic adipocytes that control energy and glucose homeostasis
J. Clin. Investig., 125 (2) (2015), pp. 478-486
View Record in ScopusGoogle Scholar[84]
W. Cao, K.W. Daniel, J. Robidoux, P. Puigserver, A.V. Medvedev, X. Bai, L.M. Floering, B.M. Spiegelman, S. Collins
p38 mitogen-activated protein kinase is the central regulator of cyclic AMP-dependent transcription of the brown fat uncoupling protein 1 gene
Mol. Cell. Biol., 24 (7) (2004), pp. 3057-3067
View Record in ScopusGoogle Scholar[85]
A. Guilherme, B. Yenilmez, A.H. Bedard, F. Henriques, D. Liu, A. Lee, L. Goldstein, M. Kelly, S.M. Nicoloro, M. Chen, L. Weinstein, S. Collins, M.P. Czech
Control of adipocyte thermogenesis and lipogenesis through β3-adrenergic and thyroid hormone signal integration
Cell reports, 31 (5) (2020), p. 107598
ArticleDownload PDFView Record in ScopusGoogle Scholar[86]
P. Seale, B. Bjork, W. Yang, S. Kajimura, S. Chin, S. Kuang, A. Scimè, S. Devarakonda, H.M. Conroe, H. Erdjument-Bromage, P. Tempst, M.A. Rudnicki, D.R. Beier, B.M. Spiegelman
PRDM16 controls a brown fat/skeletal muscle switch
Nature, 454 (7207) (2008), pp. 961-967 View PDF
CrossRefView Record in ScopusGoogle Scholar[87]
S. Carobbio, A.-C. Guenantin, M. Bahri, S. Rodriguez-Fdez, F. Honig, I. Kamzolas, I. Samuelson, K. Long, S. Awad, D. Lukovic, S. Erceg, A. Bassett, S. Mendjan, L. Vallier, B.S. Rosen, D. Chiarugi, A. Vidal-Puig
Unraveling the developmental roadmap toward human brown adipose tissue
Stem Cell Rep., 16 (3) (2021), pp. 641-655
ArticleDownload PDFView Record in ScopusGoogle Scholar[88]
Y. Oguri, K. Shinoda, H. Kim, D.L. Alba, W.R. Bolus, Q. Wang, Z. Brown, R.N. Pradhan, K. Tajima, T. Yoneshiro, K. Ikeda, Y. Chen, R.T. Cheang, K. Tsujino, C.R. Kim, V.J. Greiner, R. Datta, C.D. Yang, K. Atabai, M.T. McManus, S.K. Koliwad, B.M. Spiegelman, S. Kajimura
CD81 controls beige fat progenitor cell growth and energy balance via FAK signaling
Cell, 182 (3) (2020), pp. 563-577.e20
ArticleDownload PDFView Record in ScopusGoogle Scholar[89]
Y. Chen, K. Ikeda, T. Yoneshiro, A. Scaramozza, K. Tajima, Q. Wang, K. Kim, K. Shinoda, C.H. Sponton, Z. Brown, A. Brack, S. Kajimura
Thermal stress induces glycolytic beige fat formation via a myogenic state
Nature, 565 (7738) (2019), pp. 180-185
G. Barbatelli, I. Murano, L. Madsen, Q. Hao, M. Jimenez, K. Kristiansen, J.P. Giacobino, R. De Matteis, S. Cinti
The emergence of cold-induced brown adipocytes in mouse white fat depots is determined predominantly by white to brown adipocyte transdifferentiation, American journal of physiology
Endocrinol. Metabol., 298 (6) (2010), pp. E1244-E1253 View PDF
CrossRefView Record in ScopusGoogle Scholar[91]
A.-C. Pilkington, H.A. Paz, U.D. Wankhade
Beige Adipose Tissue Identification and Marker Specificity-Overview
Front. Endocrinol., 12 (2021), p. 599134
View Record in ScopusGoogle Scholar[92]
R.R. Stine, S.N. Shapira, H.-W. Lim, J. Ishibashi, M. Harms, K.-J. Won, P. Seale
EBF2 promotes the recruitment of beige adipocytes in white adipose tissue
Mol. Metabol., 5 (1) (2015), pp. 57-65
J. Heeren, H. Münzberg
Novel aspects of brown adipose tissue biology
Endocrinol. Metab. Clin. North Am., 42 (1) (2013), pp. 89-107
ArticleDownload PDFView Record in ScopusGoogle Scholar[94]
D. Moseti, A. Regassa, W.-K. Kim
Molecular regulation of adipogenesis and potential anti-adipogenic bioactive molecules
Int. J. Mol. Sci., 17 (1) (2016), p. 124 View PDF
CrossRefView Record in ScopusGoogle Scholar[95]
M. Lehrke, G. Pascual, C.K. Glass, M.A. Lazar
Gaining weight: the keystone symposium on PPAR and LXR
Genes Dev., 19 (15) (2005), pp. 1737-1742 View PDF
CrossRefView Record in ScopusGoogle Scholar[96]
A. Chawla, E.J. Schwarz, D.D. Dimaculangan, M.A. Lazar
Peroxisome proliferator-activated receptor (PPAR) gamma: adipose-predominant expression and induction early in adipocyte differentiation
Endocrinology, 135 (2) (1994), pp. 798-800
View Record in ScopusGoogle Scholar[97]
J.M. Lehmann, L.B. Moore, T.A. Smith-Oliver, W.O. Wilkison, T.M. Willson, S.A. Kliewer
An antidiabetic thiazolidinedione is a high affinity ligand for peroxisome proliferator-activated receptor y (PPARy)
J. Biol. Chem., 270 (22) (1995), pp. 12953-12956
ArticleDownload PDFView Record in ScopusGoogle Scholar[98]
S.R. Farmer
Transcriptional control of adipocyte formation
Cell Metab, 4 (4) (2006), pp. 263-273
ArticleDownload PDFView Record in ScopusGoogle Scholar[99]
C. Vigouroux, L. Fajas, E. Khallouf, M. Meier, G. Gyapay, O. Lascols, J. Auwerx, J. Weissenbach, J. Capeau, J. Magré
Human peroxisome proliferator-activated receptor-gamma2: genetic mapping, identification of a variant in the coding sequence, and exclusion as the gene responsible for lipoatrophic diabetes
Diabetes, 47 (3) (1998), pp. 490-492 View PDF
CrossRefView Record in ScopusGoogle Scholar[100]
E.D. Rosen, P. Sarraf, A.E. Troy, G. Bradwin, K. Moore, D.S. Milstone, B.M. Spiegelman, R.M. Mortensen
PPAR gamma is required for the differentiation of adipose tissue in vivo and in vitro
Mol Cell, 4 (4) (1999), pp. 611-617
ArticleDownload PDFView Record in ScopusGoogle Scholar[101]
R.P. Brun, P. Tontonoz, B.M. Forman, R. Ellis, J. Chen, R.M. Evans, B.M. Spiegelman
Differential activation of adipogenesis by multiple PPAR isoforms
Genes Dev, 10 (8) (1996), pp. 974-984 View PDF
CrossRefView Record in ScopusGoogle Scholar[102]
Y.X. Wang, C.H. Lee, S. Tiep, R.T. Yu, J. Ham, H. Kang, R.M. Evans
Peroxisome-proliferator-activated receptor delta activates fat metabolism to prevent obesity
Cell, 113 (2) (2003), pp. 159-170
ArticleDownload PDFView Record in ScopusGoogle Scholar[103]
J.M. Peters, S.S. Lee, W. Li, J.M. Ward, O. Gavrilova, C. Everett, M.L. Reitman, L.D. Hudson, F.J. Gonzalez
Growth, adipose, brain, and skin alterations resulting from targeted disruption of the mouse peroxisome proliferator-activated receptor beta(delta)
Mol. Cell. Biol., 20 (14) (2000), pp. 5119-5128
View Record in ScopusGoogle Scholar[104]
M. Guerre-Millo, P. Gervois, E. Raspe, L. Madsen, P. Poulain, B. Derudas, J.M. Herbert, D.A. Winegar, T.M. Willson, J.C. Fruchart, R.K. Berge, B. Staels
Peroxisome proliferator-activated receptor alpha activators improve insulin sensitivity and reduce adiposity
J. Biol. Chem., 275 (22) (2000), pp. 16638-16642
ArticleDownload PDFView Record in ScopusGoogle Scholar[105]
S. Jeong, M. Yoon
Fenofibrate inhibits adipocyte hypertrophy and insulin resistance by activating adipose PPARalpha in high fat diet-induced obese mice
Exp. Mol. Med., 41 (6) (2009), pp. 397-405
View Record in ScopusGoogle Scholar[106]
A. Tsuchida, T. Yamauchi, S. Takekawa, Y. Hada, Y. Ito, T. Maki, T. Kadowaki
Peroxisome proliferator-activated receptor (PPAR)alpha activation increases adiponectin receptors and reduces obesity-related inflammation in adipose tissue: comparison of activation of PPARalpha PPARgamma, and their combination
Diabetes, 54 (12) (2005), pp. 3358-3370 View PDF
CrossRefView Record in ScopusGoogle Scholar[107]
M. Das, M.R. Irvin, J. Sha, S. Aslibekyan, B. Hidalgo, R.T. Perry, D. Zhi, H.K. Tiwari, D. Absher, J.M. Ordovas, D.K. Arnett
Lipid changes due to fenofibrate treatment are not associated with changes in DNA methylation patterns in the GOLDN study
Front. Genet., 6 (2015), p. 304
View Record in ScopusGoogle Scholar[108]
F. Forcheron, A. Cachefo, S. Thevenon, C. Pinteur, M. Beylot
Mechanisms of the triglyceride- and cholesterol-lowering effect of fenofibrate in hyperlipidemic type 2 diabetic patients
Diabetes, 51 (12) (2002), pp. 3486-3491 View PDF
CrossRefView Record in ScopusGoogle Scholar[109]
W.R. Oliver Jr., J.L. Shenk, M.R. Snaith, C.S. Russell, K.D. Plunket, N.L. Bodkin, M.C. Lewis, D.A. Winegar, M.L. Sznaidman, M.H. Lambert, H.E. Xu, D.D. Sternbach, S.A. Kliewer, B.C. Hansen, T.M. Willson
A selective peroxisome proliferator-activated receptor delta agonist promotes reverse cholesterol transport
PNAS, 98 (9) (2001), pp. 5306-5311
C.D. Kassotis, L. Masse, S. Kim, J.J. Schlezinger, T.F. Webster, H.M. Stapleton
Characterization of adipogenic chemicals in three different cell culture systems: implications for reproducibility based on cell source and handling
Sci. Rep., 7 (2017), p. 42104
View Record in ScopusGoogle Scholar[111]
P. Tontonoz, S. Singer, B.M. Forman, P. Sarraf, J.A. Fletcher, C.D. Fletcher, R.P. Brun, E. Mueller, S. Altiok, H. Oppenheim, R.M. Evans, B.M. Spiegelman
Terminal differentiation of human liposarcoma cells induced by ligands for peroxisome proliferator-activated receptor gamma and the retinoid X receptor
PNAS, 94 (1) (1997), pp. 237-241
View Record in ScopusGoogle Scholar[112]
S.S. Canan Koch, L.J. Dardashti, R.M. Cesario, G.E. Croston, M.F. Boehm, R.A. Heyman, A.M. Nadzan
Synthesis of retinoid X receptor-specific ligands that are potent inducers of adipogenesis in 3T3-L1 cells
J Med Chem, 42 (4) (1999), pp. 742-750
R. Nielsen, T.A. Pedersen, D. Hagenbeek, P. Moulos, R. Siersbaek, E. Megens, S. Denissov, M. Borgesen, K.J. Francoijs, S. Mandrup, H.G. Stunnenberg
Genome-wide profiling of PPARgamma:RXR and RNA polymerase II occupancy reveals temporal activation of distinct metabolic pathways and changes in RXR dimer composition during adipogenesis
Genes Dev, 22 (21) (2008), pp. 2953-2967 View PDF
CrossRefView Record in ScopusGoogle Scholar[114]
B.M. Shoucri, E.S. Martinez, T.J. Abreo, V.T. Hung, Z. Moosova, T. Shioda, B. Blumberg
Retinoid X receptor activation alters the chromatin landscape to commit mesenchymal stem cells to the adipose lineage
Endocrinology, 158 (10) (2017), pp. 3109-3125 View PDF
B.M. Shoucri, V.T. Hung, R. Chamorro-García, T. Shioda, B. Blumberg
Retinoid X receptor activation during adipogenesis of female mesenchymal stem cells programs a dysfunctional adipocyte
Endocrinology, 159 (8) (2018), pp. 2863-2883 View PDF
H.M. Sucov, E. Dyson, C.L. Gumeringer, J. Price, K.R. Chien, R.M. Evans
RXR alpha mutant mice establish a genetic basis for vitamin A signaling in heart morphogenesis
Genes Dev, 8 (9) (1994), pp. 1007-1018 View PDF
CrossRefView Record in ScopusGoogle Scholar[117]
T. Imai, M. Jiang, P. Chambon, D. Metzger
Impaired adipogenesis and lipolysis in the mouse upon selective ablation of the retinoid X receptor alpha mediated by a tamoxifen-inducible chimeric Cre recombinase (Cre-ERT2) in adipocytes
PNAS, 98 (1) (2001), pp. 224-228
View Record in ScopusGoogle Scholar[118]
R. Mukherjee, P.J. Davies, D.L. Crombie, E.D. Bischoff, R.M. Cesario, L. Jow, L.G. Hamann, M.F. Boehm, C.E. Mondon, A.M. Nadzan, J.R. Paterniti Jr., R.A. Heyman
Sensitization of diabetic and obese mice to insulin by retinoid X receptor agonists
Nature, 386 (6623) (1997), pp. 407-410
View Record in ScopusGoogle Scholar[119]
M.K. Sadasivuni, B.M. Reddy, J. Singh, M.O. Anup, V. Sunil, M.N. Lakshmi, S. Yogeshwari, S.K. Chacko, T.L. Pooja, A. Dandu, C. Harish, A.S. Gopala, S. Pratibha, B.S. Naveenkumar, P.M. Pallavi, M.K. Verma, Y. Moolemath, B.P. Somesh, M.V. Venkataranganna, M.R. Jagannath
CNX-013-B2, a unique pan tissue acting rexinoid, modulates several nuclear receptors and controls multiple risk factors of the metabolic syndrome without risk of hypertriglyceridemia, hepatomegaly and body weight gain in animal models
Diabetol Metab Syndr, 6 (1) (2014), p. 83
View Record in ScopusGoogle Scholar[120]
V. Emilsson, J. O’Dowd, S. Wang, Y.L. Liu, M. Sennitt, R. Heyman, M.A. Cawthorne
The effects of rexinoids and rosiglitazone on body weight and uncoupling protein isoform expression in the Zucker fa/fa rat
Metabolism, 49 (12) (2000), pp. 1610-1615
ArticleDownload PDFView Record in ScopusGoogle Scholar[121]
L.T. Farol, K.B. Hymes
Bexarotene: a clinical review
Expert Rev. Anticancer Ther., 4 (2) (2004), pp. 180-188 View PDF
CrossRefView Record in ScopusGoogle Scholar[122]
J. de Vries-van, W. der Weij, L.H. de Haan, M. Kuif, H.L. Oei, J.W. van der Hoorn, L.M. Havekes, H.M. Princen, J.A. Romijn, J.W. Smit, P.C. Rensen
Bexarotene induces dyslipidemia by increased very low-density lipoprotein production and cholesteryl ester transfer protein-mediated reduction of high-density lipoprotein
Endocrinology, 150 (5) (2009), pp. 2368-2375
J.A. Pinaire, A. Reifel-Miller
Therapeutic potential of retinoid x receptor modulators for the treatment of the metabolic syndrome
PPAR Res, 2007 (2007), p. 94156
View Record in ScopusGoogle Scholar[124]
A.I. Shulman, D.J. Mangelsdorf
Retinoid x receptor heterodimers in the metabolic syndrome
New England J. Med., 353 (6) (2005), pp. 604-615
View Record in ScopusGoogle Scholar[125]
S.M. Ulven, K.T. Dalen, J.A. Gustafsson, H.I. Nebb
LXR is crucial in lipid metabolism
Prostaglandins Leukot Essent Fatty Acids, 73 (1) (2005), pp. 59-63
ArticleDownload PDFView Record in ScopusGoogle Scholar[126]
N.Y. Kalaany, K.C. Gauthier, A.M. Zavacki, P.P. Mammen, T. Kitazume, J.A. Peterson, J.D. Horton, D.J. Garry, A.C. Bianco, D.J. Mangelsdorf
LXRs regulate the balance between fat storage and oxidation
Cell Metab, 1 (4) (2005), pp. 231-244
ArticleDownload PDFView Record in ScopusGoogle Scholar[127]
J.B. Seo, H.M. Moon, W.S. Kim, Y.S. Lee, H.W. Jeong, E.J. Yoo, J. Ham, H. Kang, M.G. Park, K.R. Steffensen, T.M. Stulnig, J.A. Gustafsson, S.D. Park, J.B. Kim
Activated liver X receptors stimulate adipocyte differentiation through induction of peroxisome proliferator-activated receptor gamma expression
Mol. Cell Biol., 24 (8) (2004), pp. 3430-3444
View Record in ScopusGoogle Scholar[128]
L.K. Juvet, S.M. Andresen, G.U. Schuster, K.T. Dalen, K.A. Tobin, K. Hollung, F. Haugen, S. Jacinto, S.M. Ulven, K. Bamberg, J.A. Gustafsson, H.I. Nebb
On the role of liver X receptors in lipid accumulation in adipocytes
Mol. Endocrinol., 17 (2) (2003), pp. 172-182
View Record in ScopusGoogle Scholar[129]
B.M. Stenson, M. Ryden, N. Venteclef, I. Dahlman, A.M. Pettersson, A. Mairal, G. Astrom, L. Blomqvist, V. Wang, J.W. Jocken, K. Clement, D. Langin, P. Arner, J. Laurencikiene
Liver X receptor (LXR) regulates human adipocyte lipolysis
J. Biol. Chem., 286 (1) (2011), pp. 370-379
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[130]
I. Gerin, V.W. Dolinsky, J.G. Shackman, R.T. Kennedy, S.H. Chiang, C.F. Burant, K.R. Steffensen, J.A. Gustafsson, O.A. MacDougald
LXRbeta is required for adipocyte growth, glucose homeostasis, and beta cell function
J. Biol. Chem., 280 (24) (2005), pp. 23024-23031
ArticleDownload PDFView Record in ScopusGoogle Scholar[131]
M. Korach-Andre, A. Archer, R.P. Barros, P. Parini, J.A. Gustafsson
Both liver-X receptor (LXR) isoforms control energy expenditure by regulating brown adipose tissue activity
PNAS, 108 (1) (2011), pp. 403-408 View PDF
CrossRefView Record in ScopusGoogle Scholar[132]
A. Archer, E. Stolarczyk, M.L. Doria, L. Helguero, R. Domingues, J.K. Howard, A. Mode, M. Korach-Andre, J.A. Gustafsson
LXR activation by GW3965 alters fat tissue distribution and adipose tissue inflammation in ob/ob female mice
J. Lipid Res., 54 (5) (2013), pp. 1300-1311
ArticleDownload PDFView Record in ScopusGoogle Scholar[133]
I. Dahlman, M. Nilsson, H. Jiao, J. Hoffstedt, C.M. Lindgren, K. Humphreys, J. Kere, J.A. Gustafsson, P. Arner, K. Dahlman-Wright
Liver X receptor gene polymorphisms and adipose tissue expression levels in obesity
Pharmacogenet Genomics, 16 (12) (2006), pp. 881-889 View PDF
CrossRefView Record in ScopusGoogle Scholar[134]
T.G. Kirchgessner, P. Sleph, J. Ostrowski, J. Lupisella, C.S. Ryan, X. Liu, G. Fernando, D. Grimm, P. Shipkova, R. Zhang, R. Garcia, J. Zhu, A. He, H. Malone, R. Martin, K. Behnia, Z. Wang, Y.C. Barrett, R.J. Garmise, L. Yuan, J. Zhang, M.D. Gandhi, P. Wastall, T. Li, S. Du, L. Salvador, R. Mohan, G.H. Cantor, E. Kick, J. Lee, R.J. Frost
Beneficial and adverse effects of an LXR agonist on human lipid and lipoprotein metabolism and circulating neutrophils
Cell Metab, 24 (2) (2016), pp. 223-233
ArticleDownload PDFView Record in ScopusGoogle Scholar[135]
J. Gao, W. Xie
Targeting xenobiotic receptors PXR and CAR for metabolic diseases
Trends Pharmacol. Sci., 33 (10) (2012), pp. 552-558
ArticleDownload PDFView Record in ScopusGoogle Scholar[136]
A. Moreau, M.J. Vilarem, P. Maurel, J.M. Pascussi
Xenoreceptors CAR and PXR activation and consequences on lipid metabolism, glucose homeostasis, and inflammatory response
Mol. Pharm., 5 (1) (2008), pp. 35-41 View PDF
J. Zhou, M. Febbraio, T. Wada, Y. Zhai, R. Kuruba, J. He, J.H. Lee, S. Khadem, S. Ren, S. Li, R.L. Silverstein, W. Xie
Hepatic fatty acid transporter Cd36 is a common target of LXR, PXR, and PPARgamma in promoting steatosis
Gastroenterology, 134 (2) (2008), pp. 556-567
J. He, J. Gao, M. Xu, S. Ren, M. Stefanovic-Racic, R.M. O’Doherty, W. Xie
PXR ablation alleviates diet-induced and genetic obesity and insulin resistance in mice
Diabetes, 62 (6) (2013), pp. 1876-1887 View PDF
CrossRefView Record in ScopusGoogle Scholar[139]
T. Wada, J. Gao, W. Xie
PXR and CAR in energy metabolism. Trends in endocrinology and metabolism
TEM, 20 (6) (2009), pp. 273-279
ArticleDownload PDFView Record in ScopusGoogle Scholar[140]
J. Gao, J. He, Y. Zhai, T. Wada, W. Xie
The constitutive androstane receptor is an anti-obesity nuclear receptor that improves insulin sensitivity
J. Biol. Chem., 284 (38) (2009), pp. 25984-25992
ArticleDownload PDFView Record in ScopusGoogle Scholar[141]
Y. Jiao, Y. Lu, X.Y. Li
Farnesoid X receptor: a master regulator of hepatic triglyceride and glucose homeostasis
Acta Pharmacol. Sin, 36 (1) (2015), pp. 44-50 View PDF
CrossRefView Record in ScopusGoogle Scholar[142]
J. Prawitt, S. Caron, B. Staels
How to modulate FXR activity to treat the metabolic syndrome
Drug. Discov. Today: Disease Mechanisms, 6 (1–4) (2009), pp. e55-e64
ArticleDownload PDFView Record in ScopusGoogle Scholar[143]
G. Rizzo, M. Disante, A. Mencarelli, B. Renga, A. Gioiello, R. Pellicciari, S. Fiorucci
The farnesoid X receptor promotes adipocyte differentiation and regulates adipose cell function in vivo
Mol. Pharmacol., 70 (4) (2006), pp. 1164-1173 View PDF
CrossRefView Record in ScopusGoogle Scholar[144]
B. Cariou, K. van Harmelen, D. Duran-Sandoval, T.H. van Dijk, A. Grefhorst, M. Abdelkarim, S. Caron, G. Torpier, J.C. Fruchart, F.J. Gonzalez, F. Kuipers, B. Staels
The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice
J. Biol. Chem., 281 (16) (2006), pp. 11039-11049
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[145]
J.Y. Yang, M.A. Della-Fera, C.A. Baile
Guggulsterone inhibits adipocyte differentiation and induces apoptosis in 3T3-L1 cells
Obesity (Silver Spring), 16 (1) (2008), pp. 16-22 View PDF
M. Abdelkarim, S. Caron, C. Duhem, J. Prawitt, J. Dumont, A. Lucas, E. Bouchaert, O. Briand, J. Brozek, F. Kuipers, C. Fievet, B. Cariou, B. Staels
The farnesoid X receptor regulates adipocyte differentiation and function by promoting peroxisome proliferator-activated receptor-gamma and interfering with the Wnt/beta-catenin pathways
J. Biol. Chem., 285 (47) (2010), pp. 36759-36767
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[147]
J. Prawitt, M. Abdelkarim, J.H. Stroeve, I. Popescu, H. Duez, V.R. Velagapudi, J. Dumont, E. Bouchaert, T.H. van Dijk, A. Lucas, E. Dorchies, M. Daoudi, S. Lestavel, F.J. Gonzalez, M. Oresic, B. Cariou, F. Kuipers, S. Caron, B. Staels
Farnesoid X receptor deficiency improves glucose homeostasis in mouse models of obesity
Diabetes, 60 (7) (2011), pp. 1861-1871 View PDF
CrossRefView Record in ScopusGoogle Scholar[148]
Y. Zhang, X. Ge, L.A. Heemstra, W.D. Chen, J. Xu, J.L. Smith, H. Ma, N. Kasim, P.A. Edwards, C.M. Novak
Loss of FXR protects against diet-induced obesity and accelerates liver carcinogenesis in ob/ob mice
Mol. Endocrinol., 26 (2) (2012), pp. 272-280 View PDF
CrossRefView Record in ScopusGoogle Scholar[149]
E. Maneschi, L. Vignozzi, A. Morelli, T. Mello, S. Filippi, I. Cellai, P. Comeglio, E. Sarchielli, A. Calcagno, B. Mazzanti, R. Vettor, G.B. Vannelli, L. Adorini, M. Maggi
FXR activation normalizes insulin sensitivity in visceral preadipocytes of a rabbit model of MetS
J. Endocrinol., 218 (2) (2013), pp. 215-231
View Record in ScopusGoogle Scholar[150]
M. Watanabe, Y. Horai, S.M. Houten, K. Morimoto, T. Sugizaki, E. Arita, C. Mataki, H. Sato, Y. Tanigawara, K. Schoonjans, H. Itoh, J. Auwerx
Lowering bile acid pool size with a synthetic farnesoid X receptor (FXR) agonist induces obesity and diabetes through reduced energy expenditure
J. Biol. Chem., 286 (30) (2011), pp. 26913-26920
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[151]
D.J. Rader
Liver X receptor and farnesoid X receptor as therapeutic targets
Am. J. Cardiol., 100 (11A) (2007), pp. 15N-19N
Y. Lu, Z. Ma, Z. Zhang, X. Xiong, X. Wang, H. Zhang, G. Shi, X. Xia, G. Ning, X. Li
Yin Yang 1 promotes hepatic steatosis through repression of farnesoid X receptor in obese mice
Gut, 63 (1) (2014), pp. 170-178
B.E. McIntosh, J.B. Hogenesch, C.A. Bradfield
Mammalian Per-Arnt-Sim proteins in environmental adaptation
Annu. Rev. Physiol., 72 (2010), pp. 625-645 View PDF
CrossRefView Record in ScopusGoogle Scholar[154]
D.C. de Almeida, L.S.M. Evangelista, N.O.S. Câmara
Role of aryl hydrocarbon receptor in mesenchymal stromal cell activation: a minireview
World J. Stem. Cells, 9 (9) (2017), pp. 152-158
View Record in ScopusGoogle Scholar[155]
C.J. Henderson, L.A. McLaughlin, M. Osuna-Cabello, M. Taylor, I. Gilbert, A.W. McLaren, C.R. Wolf
Application of a novel regulatable Cre recombinase system to define the role of liver and gut metabolism in drug oral bioavailability
Biochem. J, 465 (3) (2015), pp. 479-488
View Record in ScopusGoogle Scholar[156]
Y. Shimizu, Y. Nakatsuru, M. Ichinose, Y. Takahashi, H. Kume, J. Mimura, Y. Fujii-Kuriyama, T. Ishikawa
Benzo[a]pyrene carcinogenicity is lost in mice lacking the aryl hydrocarbon receptor
Proc. Natl. Acad. Sci., 97 (2) (2000), pp. 779-782
View Record in ScopusGoogle Scholar[157]
P. Nguyen, V. Leray, M. Diez, S. Serisier, J. Le Bloc’h, B. Siliart, H. Dumon
Liver lipid metabolism
J. Anim. Physiol. Anim. Nutrit., 92 (3) (2008), pp. 272-283 View PDF
CrossRefView Record in ScopusGoogle Scholar[158]
R. Tanos, R.D. Patel, I.A. Murray, P.B. Smith, A.D. Patterson, G.H. Perdew
Aryl hydrocarbon receptor regulates the cholesterol biosynthetic pathway in a dioxin response element-independent manner
Hepatology (Baltimore Md.), 55 (6) (2012), pp. 1994-2004 View PDF
CrossRefView Record in ScopusGoogle Scholar[159]
R. Tanos, I.A. Murray, P.B. Smith, A. Patterson, G.H. Perdew
Role of the Ah receptor in homeostatic control of fatty acid synthesis in the liver
Toxicol. Sci.: Off. J. Soc. Toxicol., 129 (2) (2012), pp. 372-379 View PDF
CrossRefView Record in ScopusGoogle Scholar[160]
N.G. Girer, D. Carter, N. Bhattarai, M. Mustafa, L. Denner, C. Porter, C.J. Elferink
Inducible loss of the aryl hydrocarbon receptor activates perigonadal white fat respiration and brown fat thermogenesis via fibroblast growth factor 21
Int. J. Mol. Sci., 20 (4) (2019)
J. Beltrand, K. Busiah, L. Vaivre-Douret, A.L. Fauret, M. Berdugo, H. Cavé, M. Polak
Neonatal diabetes mellitus
Front Pediatr, 8 (2020), p. 540718
View Record in ScopusGoogle Scholar[162]
M. Plamper, B. Gohlke, F. Schreiner, J. Woelfle
Mecasermin in insulin receptor-related severe insulin resistance syndromes: case report and review of the literature
Int. J. Mol. Sci., 19 (5) (2018), p. 1268 View PDF
CrossRefView Record in ScopusGoogle Scholar[163]
J. Boucher, S. Softic, A. El Ouaamari, M.T. Krumpoch, A. Kleinridders, R.N. Kulkarni, B.T. O’Neill, C.R. Kahn
Differential roles of insulin and IGF-1 receptors in adipose tissue development and function
Diabetes, 65 (8) (2016), pp. 2201-2213 View PDF
CrossRefView Record in ScopusGoogle Scholar[164]
E.P. Homan, B.B. Brandão, S. Softic, A. El Ouaamari, B.T. O’Neill, R.N. Kulkarni, J.K. Kim, C.R. Kahn
Differential roles of FOXO transcription factors on insulin action in brown and white adipose tissue
J. Clin. Invest., 131 (19) (2021)
A. Nadal, A.B. Ropero, O. Laribi, M. Maillet, E. Fuentes, B. Soria
Nongenomic actions of estrogens and xenoestrogens by binding at a plasma membrane receptor unrelated to estrogen receptor alpha and estrogen receptor beta
PNAS, 97 (21) (2000), pp. 11603-11608
View Record in ScopusGoogle Scholar[166]
N. Fuentes, P. Silveyra
Estrogen receptor signaling mechanisms
Adv. Protein. Chem. Struct. Biol., 116 (2019), pp. 135-170
ArticleDownload PDFView Record in ScopusGoogle Scholar[167]
C.B. Jasik, R.H. Lustig
Adolescent obesity and puberty: the “perfect storm”
Ann. N Y Acad. Sci., 1135 (2008), pp. 265-279 View PDF
CrossRefView Record in ScopusGoogle Scholar[168]
M.K. Crocker, E.A. Stern, N.M. Sedaka, L.B. Shomaker, S.M. Brady, A.H. Ali, T.H. Shawker, V.S. Hubbard, J.A. Yanovski
Sexual dimorphisms in the associations of BMI and body fat with indices of pubertal development in girls and boys
J. Clin. Endocrinol. Metabol., 99 (8) (2014), pp. E1519-E1529 View PDF
CrossRefView Record in ScopusGoogle Scholar[169]
S.R. Davis, C. Castelo-Branco, P. Chedraui, M.A. Lumsden, R.E. Nappi, D. Shah, P. Villaseca
Understanding weight gain at menopause
Climacteric, 15 (2012), pp. 419-429 View PDF
CrossRefView Record in ScopusGoogle Scholar[170]
P.S. Cooke, A. Naaz
Role of estrogens in adipocyte development and function
Exp. Biol. Med. (Maywood), 229 (11) (2004), pp. 1127-1135 View PDF
CrossRefView Record in ScopusGoogle Scholar[171]
M.N. Dieudonne, R. Pecquery, M.C. Leneveu, Y. Giudicelli
Opposite effects of androgens and estrogens on adipogenesis in rat preadipocytes: evidence for sex and site-related specificities and possible involvement of insulin-like growth factor 1 receptor and peroxisome proliferator-activated receptor gamma2
Endocrinology, 141 (2) (2000), pp. 649-656
View Record in ScopusGoogle Scholar[172]
D.A. Roncari, R.L. Van
Promotion of human adipocyte precursor replication by 17beta-estradiol in culture
J. Clin. Invest., 62 (3) (1978), pp. 503-508 View PDF
CrossRefView Record in ScopusGoogle Scholar[173]
P.A. Heine, J.A. Taylor, G.A. Iwamoto, D.B. Lubahn, P.S. Cooke
Increased adipose tissue in male and female estrogen receptor-alpha knockout mice
PNAS, 97 (23) (2000), pp. 12729-12734
View Record in ScopusGoogle Scholar[174]
C. Ohlsson, N. Hellberg, P. Parini, O. Vidal, Y.M. Bohlooly, M. Rudling, M.K. Lindberg, M. Warner, B. Angelin, J.A. Gustafsson
Obesity and disturbed lipoprotein profile in estrogen receptor-alpha-deficient male mice
Biochem. Biophys. Res. Commun., 278 (3) (2000), pp. 640-645
ArticleDownload PDFView Record in ScopusGoogle Scholar[175]
R.E. Stubbins, V.B. Holcomb, J. Hong, N.P. Nunez
Estrogen modulates abdominal adiposity and protects female mice from obesity and impaired glucose tolerance
Eur. J. Nutr., 51 (7) (2012), pp. 861-870 View PDF
CrossRefView Record in ScopusGoogle Scholar[176]
Y. Murata, K.M. Robertson, M.E. Jones, E.R. Simpson
Effect of estrogen deficiency in the male: the ArKO mouse model
Mol. Cell Endocrinol., 193 (1–2) (2002), pp. 7-12
ArticleDownload PDFView Record in ScopusGoogle Scholar[177]
M.E. Jones, A.W. Thorburn, K.L. Britt, K.N. Hewitt, M.L. Misso, N.G. Wreford, J. Proietto, O.K. Oz, B.J. Leury, K.M. Robertson, S. Yao, E.R. Simpson
Aromatase-deficient (ArKO) mice accumulate excess adipose tissue
J. Steroid. Biochem. Mol. Biol., 79 (1–5) (2001), pp. 3-9
ArticleDownload PDFView Record in ScopusGoogle Scholar[178]
M.E. Jones, A.W. Thorburn, K.L. Britt, K.N. Hewitt, N.G. Wreford, J. Proietto, O.K. Oz, B.J. Leury, K.M. Robertson, S. Yao, E.R. Simpson
Aromatase-deficient (ArKO) mice have a phenotype of increased adiposity
PNAS, 97 (23) (2000), pp. 12735-12740
View Record in ScopusGoogle Scholar[179]
L. Hong, A. Colpan, I.A. Peptan
Modulations of 17-beta estradiol on osteogenic and adipogenic differentiations of human mesenchymal stem cells
Tissue Eng, 12 (10) (2006), pp. 2747-2753 View PDF
CrossRefView Record in ScopusGoogle Scholar[180]
P. Zhu, J.M. Yuen, K.W. Sham, C.H. Cheng
GPER mediates the inhibitory actions of estrogen on adipogenesis in 3T3-L1 cells through perturbation of mitotic clonal expansion
Gen. Comp. Endocrinol., 193 (2013), pp. 19-26
ArticleDownload PDFView Record in ScopusGoogle Scholar[181]
K. Blouin, A. Boivin, A. Tchernof
Androgens and body fat distribution
J. Steroid. Biochem. Mol. Biol., 108 (3–5) (2008), pp. 272-280
ArticleDownload PDFView Record in ScopusGoogle Scholar[182]
M.W. O’Reilly, P.J. House, J.W. Tomlinson
Understanding androgen action in adipose tissue
J. Steroid. Biochem. Mol. Biol., 143 (2014), pp. 277-284
ArticleDownload PDFView Record in ScopusGoogle Scholar[183]
V. Gupta, S. Bhasin, W. Guo, R. Singh, R. Miki, P. Chauhan, K. Choong, T. Tchkonia, N.K. Lebrasseur, J.N. Flanagan, J.A. Hamilton, J.C. Viereck, N.S. Narula, J.L. Kirkland, R. Jasuja
Effects of dihydrotestosterone on differentiation and proliferation of human mesenchymal stem cells and preadipocytes
Mol. Cell Endocrinol., 296 (1–2) (2008), pp. 32-40
ArticleDownload PDFView Record in ScopusGoogle Scholar[184]
G. Chazenbalk, P. Singh, D. Irge, A. Shah, D.H. Abbott, D.A. Dumesic
Androgens inhibit adipogenesis during human adipose stem cell commitment to preadipocyte formation
Steroids, 78 (9) (2013), pp. 920-926
ArticleDownload PDFView Record in ScopusGoogle Scholar[185]
R. Singh, J.N. Artaza, W.E. Taylor, N.F. Gonzalez-Cadavid, S. Bhasin
Androgens stimulate myogenic differentiation and inhibit adipogenesis in C3H 10T1/2 pluripotent cells through an androgen receptor-mediated pathway
Endocrinology, 144 (11) (2003), pp. 5081-5088
View Record in ScopusGoogle Scholar[186]
T. Sato, T. Matsumoto, T. Yamada, T. Watanabe, H. Kawano, S. Kato
Late onset of obesity in male androgen receptor-deficient (AR KO) mice
Biochem. Biophys. Res. Commun., 300 (1) (2003), pp. 167-171
ArticleDownload PDFView Record in ScopusGoogle Scholar[187]
T. Yanase, W. Fan, K. Kyoya, L. Min, R. Takayanagi, S. Kato, H. Nawata
Androgens and metabolic syndrome: lessons from androgen receptor knock out (ARKO) mice
J. Steroid. Biochem. Mol. Biol., 109 (3–5) (2008), pp. 254-257
ArticleDownload PDFView Record in ScopusGoogle Scholar[188]
J.B. Fagman, A.S. Wilhelmson, B.M. Motta, C. Pirazzi, C. Alexanderson, K. De Gendt, G. Verhoeven, A. Holmang, F. Anesten, J.O. Jansson, M. Levin, J. Boren, C. Ohlsson, A. Krettek, S. Romeo, A. Tivesten
The androgen receptor confers protection against diet-induced atherosclerosis, obesity, and dyslipidemia in female mice
FASEB J.: Off. Publicat. Federat. Am. Soc. Exp. Biol., 29 (4) (2015), pp. 1540-1550 View PDF
CrossRefView Record in ScopusGoogle Scholar[189]
S. Yeh, M.Y. Tsai, Q. Xu, X.M. Mu, H. Lardy, K.E. Huang, H. Lin, S.D. Yeh, S. Altuwaijri, X. Zhou, L. Xing, B.F. Boyce, M.C. Hung, S. Zhang, L. Gan, C. Chang
Generation and characterization of androgen receptor knockout (ARKO) mice: an in vivo model for the study of androgen functions in selective tissues
PNAS, 99 (21) (2002), pp. 13498-13503
View Record in ScopusGoogle Scholar[190]
W. Fan, T. Yanase, M. Nomura, T. Okabe, K. Goto, T. Sato, H. Kawano, S. Kato, H. Nawata
Androgen receptor null male mice develop late-onset obesity caused by decreased energy expenditure and lipolytic activity but show normal insulin sensitivity with high adiponectin secretion
Diabetes, 54 (4) (2005), pp. 1000-1008 View PDF
CrossRefView Record in ScopusGoogle Scholar[191]
K. Blouin, M. Nadeau, M. Perreault, A. Veilleux, R. Drolet, P. Marceau, J. Mailloux, V. Luu-The, A. Tchernof
Effects of androgens on adipocyte differentiation and adipose tissue explant metabolism in men and women
Clin. Endocrinol., 72 (2) (2010), pp. 176-188 View PDF
CrossRefView Record in ScopusGoogle Scholar[192]
C. Mammi, M. Calanchini, A. Antelmi, F. Cinti, G.M. Rosano, A. Lenzi, M. Caprio, A. Fabbri
Androgens and adipose tissue in males: a complex and reciprocal interplay
Int. J. Endocrinol., 2012 (2012), Article 789653
View Record in ScopusGoogle Scholar[193]
E. Diamanti-Kandarakis, A. Mitrakou, S. Raptis, G. Tolis, A.J. Duleba
The effect of a pure antiandrogen receptor blocker, flutamide, on the lipid profile in the polycystic ovary syndrome
J. Clin. Endocrinol. Metabol., 83 (8) (1998), pp. 2699-2705
View Record in ScopusGoogle Scholar[194]
L. Ibanez, K. Ong, A. Ferrer, R. Amin, D. Dunger, F. de Zegher
Low-dose flutamide-metformin therapy reverses insulin resistance and reduces fat mass in nonobese adolescents with ovarian hyperandrogenism
J. Clin. Endocrinol. Metabol., 88 (6) (2003), pp. 2600-2606
View Record in ScopusGoogle Scholar[195]
L. Ibanez, F. De Zegher
Flutamide-metformin therapy to reduce fat mass in hyperinsulinemic ovarian hyperandrogenism: effects in adolescents and in women on third-generation oral contraception
J. Clin. Endocrinol. Metabol., 88 (10) (2003), pp. 4720-4724
View Record in ScopusGoogle Scholar[196]
R. Pasquali
Obesity and androgens: facts and perspectives
Fertil Steril, 85 (5) (2006), pp. 1319-1340
ArticleDownload PDFView Record in ScopusGoogle Scholar[197]
B.J. Feldman
Glucocorticoids influence on mesenchymal stem cells and implications for metabolic disease
Pediatr Res, 65 (2) (2009), pp. 249-251 View PDF
B.R. Walker, S. Soderberg, B. Lindahl, T. Olsson
Independent effects of obesity and cortisol in predicting cardiovascular risk factors in men and women
J. Intern. Med., 247 (2) (2000), pp. 198-204
View Record in ScopusGoogle Scholar[199]
R.T. Pickering, M.J. Lee, K. Karastergiou, A. Gower, S.K. Fried
Depot dependent effects of dexamethasone on gene expression in human omental and abdominal subcutaneous adipose tissues from obese women
PLoS ONE, 11 (12) (2016), Article e0167337 View PDF
CrossRefView Record in ScopusGoogle Scholar[200]
E.B. Geer, W. Shen, E. Strohmayer, K.D. Post, P.U. Freda
Body composition and cardiovascular risk markers after remission of Cushing’s disease: a prospective study using whole-body MRI
J. Clin. Endocrinol. Metabol., 97 (5) (2012), pp. 1702-1711 View PDF
CrossRefView Record in ScopusGoogle Scholar[201]
H. Masuzaki, J. Paterson, H. Shinyama, N.M. Morton, J.J. Mullins, J.R. Seckl, J.S. Flier
A transgenic model of visceral obesity and the metabolic syndrome
Science, 294 (5549) (2001), pp. 2166-2170
View Record in ScopusGoogle Scholar[202]
K. John, J.S. Marino, E.R. Sanchez, T.D. Hinds Jr.
The glucocorticoid receptor: cause of or cure for obesity?
Am. J. Physiol. Endocrinol. Metabol., 310 (4) (2016), pp. E249-E257 View PDF
CrossRefView Record in ScopusGoogle Scholar[203]
D. Contador, F. Ezquer, M. Espinosa, M. Arango-Rodriguez, C. Puebla, L. Sobrevia, P. Conget
Dexamethasone and rosiglitazone are sufficient and necessary for producing functional adipocytes from mesenchymal stem cells
Exp. Biol. Med. (Maywood), 240 (9) (2015), pp. 1235-1246 View PDF
CrossRefView Record in ScopusGoogle Scholar[204]
M. Asada, A. Rauch, H. Shimizu, H. Maruyama, S. Miyaki, M. Shibamori, H. Kawasome, H. Ishiyama, J. Tuckermann, H. Asahara
DNA binding-dependent glucocorticoid receptor activity promotes adipogenesis via Kruppel-like factor 15 gene expression
Lab. Invest., 91 (2) (2011), pp. 203-215 View PDF
CrossRefView Record in ScopusGoogle Scholar[205]
A.J. Vidal-Puig, R.V. Considine, M. Jimenez-Linan, A. Werman, W.J. Pories, J.F. Caro, J.S. Flier
Peroxisome proliferator-activated receptor gene expression in human tissues. Effects of obesity, weight loss, and regulation by insulin and glucocorticoids
J. Clin. Invest., 99 (10) (1997), pp. 2416-2422 View PDF
CrossRefView Record in ScopusGoogle Scholar[206]
R.M. Sargis, D.N. Johnson, R.A. Choudhury, M.J. Brady
Environmental endocrine disruptors promote adipogenesis in the 3T3-L1 cell line through glucocorticoid receptor activation
Obesity (Silver Spring Md.), 18 (7) (2010), pp. 1283-1288 View PDF
CrossRefView Record in ScopusGoogle Scholar[207]M.J. Lee, S.K. Fried, The glucocorticoid receptor, not the mineralocorticoid receptor, plays the dominant role in adipogenesis and adipokine production in human adipocytes, Int. J. Obesity (2005) 38(9) (2014) 1228-33.
C. Pantoja, J.T. Huff, K.R. Yamamoto
Glucocorticoid signaling defines a novel commitment state during adipogenesis in vitro
Mol. Biol. Cell, 19 (10) (2008), pp. 4032-4041
View Record in ScopusGoogle Scholar[209]
S. Whirledge, D.B. DeFranco
Glucocorticoid signaling in health and disease: insights from tissue-specific GR knockout mice
Endocrinol., 159 (1) (2018), pp. 46-64 View PDF
E.E. Kershaw, N.M. Morton, H. Dhillon, L. Ramage, J.R. Seckl, J.S. Flier
Adipocyte-specific glucocorticoid inactivation protects against diet-induced obesity
Diabetes, 54 (4) (2005), pp. 1023-1031 View PDF
CrossRefView Record in ScopusGoogle Scholar[211]
K.A. Iwen, E. Schroder, G. Brabant
Thyroid hormones and the metabolic syndrome
Eur. Thyroid J., 2 (2) (2013), pp. 83-92 View PDF
CrossRefView Record in ScopusGoogle Scholar[212]
M.J. Obregon
Thyroid hormone and adipocyte differentiation
Thyroid, 18 (2) (2008), pp. 185-195 View PDF
CrossRefView Record in ScopusGoogle Scholar[213]
C. Darimont, D. Gaillard, G. Ailhaud, R. Negrel
Terminal differentiation of mouse preadipocyte cells: adipogenic and antimitogenic role of triiodothyronine
Mol. Cell Endocrinol., 98 (1) (1993), pp. 67-73
ArticleDownload PDFView Record in ScopusGoogle Scholar[214]
W. Jiang, T. Miyamoto, T. Kakizawa, T. Sakuma, S. Nishio, T. Takeda, S. Suzuki, K. Hashizume
Expression of thyroid hormone receptor alpha in 3T3-L1 adipocytes; triiodothyronine increases the expression of lipogenic enzyme and triglyceride accumulation
J. Endocrinol., 182 (2) (2004), pp. 295-302 View PDF
CrossRefView Record in ScopusGoogle Scholar[215]
P. Pelletier, K. Gauthier, O. Sideleva, J. Samarut, J.E. Silva
Mice lacking the thyroid hormone receptor-alpha gene spend more energy in thermogenesis, burn more fat, and are less sensitive to high-fat diet-induced obesity
Endocrinology, 149 (12) (2008), pp. 6471-6486 View PDF
CrossRefView Record in ScopusGoogle Scholar[216]
Y.Y. Liu, J.J. Schultz, G.A. Brent
A thyroid hormone receptor alpha gene mutation (P398H) is associated with visceral adiposity and impaired catecholamine-stimulated lipolysis in mice
J. Biol. Chem., 278 (40) (2003), pp. 38913-38920
ArticleDownload PDFView Record in ScopusGoogle Scholar[217]
R.E. Weiss, Y. Murata, K. Cua, Y. Hayashi, H. Seo, S. Refetoff
Thyroid hormone action on liver, heart, and energy expenditure in thyroid hormone receptor beta-deficient mice
Endocrinology, 139 (12) (1998), pp. 4945-4952
View Record in ScopusGoogle Scholar[218]
C. Lu, S.Y. Cheng
Thyroid hormone receptors regulate adipogenesis and carcinogenesis via crosstalk signaling with peroxisome proliferator-activated receptors
J. Mol. Endocrinol., 44 (3) (2010), pp. 143-154 View PDF
CrossRefView Record in ScopusGoogle Scholar[219]
G.J. Grover, K. Mellstrom, J. Malm
Therapeutic potential for thyroid hormone receptor-beta selective agonists for treating obesity, hyperlipidemia and diabetes
Curr. Vasc. Pharmacol., 5 (2) (2007), pp. 141-154 View PDF
CrossRefView Record in ScopusGoogle Scholar[220]
G. Bryzgalova, S. Effendic, A. Khan, S. Rehnmark, P. Barbounis, J. Boulet, G. Dong, R. Singh, S. Shapses, J. Malm, P. Webb, J.D. Baxter, G.J. Grover
Anti-obesity, anti-diabetic, and lipid lowering effects of the thyroid receptor beta subtype selective agonist KB-141
J. Steroid. Biochem. Mol. Biol., 111 (3–5) (2008), pp. 262-267
ArticleDownload PDFView Record in ScopusGoogle Scholar[221]
J. Dale, J. Daykin, R. Holder, M.C. Sheppard, J.A. Franklyn
Weight gain following treatment of hyperthyroidism
Clin. Endocrinol., 55 (2) (2001), pp. 233-239
View Record in ScopusGoogle Scholar[222]
L. Lonn, K. Stenlof, M. Ottosson, A.K. Lindroos, E. Nystrom, L. Sjostrom
Body weight and body composition changes after treatment of hyperthyroidism
J. Clin. Endocrinol. Metabol., 83 (12) (1998), pp. 4269-4273
View Record in ScopusGoogle Scholar[223]U. Kolyvanos Naumann, J. Furer, L. Kaser, W. Vetter, [Hypothyroidism. Main symptoms: fatigue, weight gain, depression, myalgia, edema], Praxis (Bern 1994) 96(38) (2007) 1411-7.
P. Bratusch-Marrain, P. Schmid, W. Waldhausl, W. Schlick
Specific weight loss in hyperthyroidism
Horm. Metab. Res., 10 (5) (1978), pp. 412-415 View PDF
CrossRefView Record in ScopusGoogle Scholar[225]
E. Valassi, M. Scacchi, F. Cavagnini
Neuroendocrine control of food intake
Nutr. Metab. Cardiovasc. Dis., 18 (2) (2008), pp. 158-168
ArticleDownload PDFView Record in ScopusGoogle Scholar[226]
J.W. Sohn
Network of Hypothalamic Neurons that Control Appetite
BMB reports (2015)
M.A. Rossi, G.D. Stuber
Overlapping brain circuits for homeostatic and hedonic feeding
Cell Metab., 27 (1) (2018), pp. 42-56
ArticleDownload PDFView Record in ScopusGoogle Scholar[228]
M. Lutter, E.J. Nestler
Homeostatic and hedonic signals interact in the regulation of food intake
J. Nutrit., 139 (3) (2009), pp. 629-632 View PDF
CrossRefView Record in ScopusGoogle Scholar[229]
P. Matafome, R. Seiça
The role of brain in energy balance
Adv Neurobiol, 19 (2017), pp. 33-48 View PDF
CrossRefView Record in ScopusGoogle Scholar[230]
L.K. Heisler, D.D. Lam
An appetite for life: brain regulation of hunger and satiety
Curr. Opin. Pharmacol., 37 (2017), pp. 100-106
ArticleDownload PDFView Record in ScopusGoogle Scholar[231]
C. Koliaki, S. Liatis, M. Dalamaga, A. Kokkinos
The implication of gut hormones in the regulation of energy homeostasis and their role in the pathophysiology of obesity
Curr. Obes. Rep., 9 (3) (2020), pp. 255-271 View PDF
CrossRefView Record in ScopusGoogle Scholar[232]
G.J. Morton, T.H. Meek, M.W. Schwartz
Neurobiology of food intake in health and disease
Nat. Rev. Neurosci., 15 (6) (2014), pp. 367-378 View PDF
CrossRefView Record in ScopusGoogle Scholar[233]
A. Kleinridders, H.A. Ferris, W. Cai, C.R. Kahn
Insulin action in brain regulates systemic metabolism and brain function
Diabetes, 63 (7) (2014), pp. 2232-2243 View PDF
CrossRefView Record in ScopusGoogle Scholar[234]
T.L. Stincic, O.K. Rønnekleiv, M.J. Kelly
Diverse actions of estradiol on anorexigenic and orexigenic hypothalamic arcuate neurons
Horm. Behav., 104 (2018), pp. 146-155
ArticleDownload PDFView Record in ScopusGoogle Scholar[235]
D. Zanchi, A. Depoorter, L. Egloff, S. Haller, L. Mählmann, U.E. Lang, J. Drewe, C. Beglinger, A. Schmidt, S. Borgwardt
The impact of gut hormones on the neural circuit of appetite and satiety: a systematic review
Neurosci. Biobehav. Rev., 80 (2017), pp. 457-475
ArticleDownload PDFView Record in ScopusGoogle Scholar[236]
M.C. Makris, A. Alexandrou, E.G. Papatsoutsos, G. Malietzis, D.I. Tsilimigras, A.D. Guerron, D. Moris
Ghrelin and obesity: identifying gaps and dispelling myths
A Reappraisal, In Vivo, 31 (6) (2017), pp. 1047-1050
View Record in ScopusGoogle Scholar[237]
R.M. Kessler, P.H. Hutson, B.K. Herman, M.N. Potenza
Neuroscience and biobehavioral reviews the neurobiological basis of binge-eating disorder
Neurosci. Biobehav. Rev., 63 (2016), pp. 223-238
ArticleDownload PDFView Record in ScopusGoogle Scholar[238]
J.H. Baik
Dopamine signaling in reward-related behaviors
Front Neural Circuits, 7 (2013), p. 152
View Record in ScopusGoogle Scholar[239]
J.H. Baik
Dopaminergic control of the feeding circuit
Endocrinol. Metab. (Seoul), 36 (2) (2021), pp. 229-239 View PDF
CrossRefView Record in ScopusGoogle Scholar[240]
D.A. Wiss, K. Criscitelli, M. Gold, N. Avena
Preclinical evidence for the addiction potential of highly palatable foods: current developments related to maternal influence
Appetite, 115 (2017), pp. 19-27
ArticleDownload PDFView Record in ScopusGoogle Scholar[241]
P. Charbogne, O. Gardon, E. Martín-García, H.L. Keyworth, A. Matsui, A.E. Mechling, T. Bienert, M.T. Nasseef, A. Robé, L. Moquin, E. Darcq, S. Ben Hamida, P. Robledo, A. Matifas, K. Befort, C. Gavériaux-Ruff, L.A. Harsan, D. von Elverfeldt, J. Hennig, A. Gratton, I. Kitchen, A. Bailey, V.A. Alvarez, R. Maldonado, B.L. Kieffer
Mu opioid receptors in gamma-aminobutyric acidergic forebrain neurons moderate motivation for heroin and palatable food
Biol. Psychiatry, 81 (9) (2017), pp. 778-788
ArticleDownload PDFView Record in ScopusGoogle Scholar[242]
M. Rosenbaum, E.M. Murphy, S.B. Heymsfield, D.E. Matthews, R.L. Leibel
Low dose leptin administration reverses effects of sustained weight-reduction on energy expenditure and circulating concentrations of thyroid hormones
J. Clin. Endocrinol. Metabol., 87 (5) (2002), pp. 2391-2394 View PDF
CrossRefView Record in ScopusGoogle Scholar[243]
Y.H. Yu, J.R. Vasselli, Y. Zhang, J.I. Mechanick, J. Korner, R. Peterli
Metabolic vs. hedonic obesity: a conceptual distinction and its clinical implications
Obes. Rev., 16 (3) (2015), pp. 234-247 View PDF
Y.H. Yu
Making sense of metabolic obesity and hedonic obesity
J. Diabetes, 9 (7) (2017), pp. 656-666 View PDF
CrossRefView Record in ScopusGoogle Scholar[245]
R.H. Lustig, S. Sen, J.E. Soberman, P.A. Velasquez-Mieyer
Obesity, leptin resistance, and the effects of insulin reduction
Int. J. Obesity Related Metabol. Disorders: J. Int. Assoc. Study Obesity, 28 (10) (2004), pp. 1344-1348 View PDF
CrossRefView Record in ScopusGoogle Scholar[246]
I.S. Farooqi, E. Bullmore, J. Keogh, J. Gillard, S. O’Rahilly, P.C. Fletcher
Leptin regulates striatal regions and human eating behavior
Science, 317 (5843) (2007), p. 1355 View PDF
H. Münzberg, M.G. Myers Jr.
Molecular and anatomical determinants of central leptin resistance
Nat. Neurosci., 8 (5) (2005), pp. 566-570 View PDF
CrossRefView Record in ScopusGoogle Scholar[248]
D.P. Figlewicz, S.B. Evans, J. Murphy, M. Hoen, D.G. Baskin
Expression of receptors for insulin and leptin in the ventral tegmental area/substantia nigra (VTA/SN) of the rat
Brain Res., 964 (1) (2003), pp. 107-115
ArticleDownload PDFView Record in ScopusGoogle Scholar[249]
J.W. Hill, K.W. Williams, C. Ye, J. Luo, N. Balthasar, R. Coppari, M.A. Cowley, L.C. Cantley, B.B. Lowell, J.K. Elmquist
Acute effects of leptin require PI3K signaling in hypothalamic proopiomelanocortin neurons in mice
J. Clin. Invest., 118 (5) (2008), pp. 1796-1805
View Record in ScopusGoogle Scholar[250]
X. Lin, A. Taguchi, S. Park, J.A. Kushner, F. Li, Y. Li, M.F. White
Dysregulation of insulin receptor substrate 2 in beta cells and brain causes obesity and diabetes
J. Clin. Invest., 114 (7) (2004), pp. 908-916
View Record in ScopusGoogle Scholar[251]
J.M. Zabolotny, K.K. Bence-Hanulec, A. Stricker-Krongrad, F. Haj, Y. Wang, Y. Minokoshi, Y.B. Kim, J.K. Elmquist, L.A. Tartaglia, B.B. Kahn, B.G. Neel
PTP1B regulates leptin signal transduction in vivo
Dev. Cell, 2 (4) (2002), pp. 489-495
ArticleDownload PDFView Record in ScopusGoogle Scholar[252]
R.H. Lustig
Childhood obesity: behavioral aberration or biochemical drive? Reinterpreting the first law of thermodynamics
Nat. Clin. Pract. Endocrinol. Metab., 2 (8) (2006), pp. 447-458 View PDF
CrossRefView Record in ScopusGoogle Scholar[253]
M.L. Mietus-Snyder, R.H. Lustig
Childhood obesity: adrift in the “limbic triangle”
Annu. Rev. Med., 59 (2008), pp. 147-162 View PDF
CrossRefView Record in ScopusGoogle Scholar[254]
C.M. Aguilera, J. Olza, A. Gil
Genetic susceptibility to obesity and metabolic syndrome in childhood
Nutr. Hosp., 28 (Suppl 5) (2013), pp. 44-55
View Record in ScopusGoogle Scholar[255]
A.J. Lusis, A.D. Attie, K. Reue
Metabolic syndrome: from epidemiology to systems biology
Nat. Rev. Genet., 9 (11) (2008), pp. 819-830 View PDF
CrossRefView Record in ScopusGoogle Scholar[256]
D.S. Ludwig, L.J. Aronne, A. Astrup, R. de Cabo, L.C. Cantley, M.I. Friedman, S.B. Heymsfield, J.D. Johnson, J.C. King, R.M. Krauss, D.E. Lieberman, G. Taubes, J.S. Volek, E.C. Westman, W.C. Willett, W.S. Yancy, C.B. Ebbeling
The carbohydrate-insulin model: a physiological perspective on the obesity pandemic
Am. J. Clin. Nutr. (2021)
Google Scholar[257]K.L. Stanhope, M.I. Goran, A. Bosy-Westphal, e. al., Pathways and mechanisms linking dietary components to cardiometabolic disease: thinking beyond calories, Obes. Rev. 19(9) (2018) 1205-1295.
M.O. Weickert, A.F.H. Pfeiffer
Metabolic effects of dietary fiber consumption and prevention of diabetes
J. Nutr., 138 (2008), pp. 439-442 View PDF
CrossRefGoogle Scholar[259]M.S. Desai, A.M. Seekatz, N.M. Koropatkin, e. al., A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility, Cell 167(5) (2016) 1339–1353.e21.
R. Ferrarese, E.R. Ceresola, A. Preti, F. Canducci
Probiotics, prebiotics and synbiotics for weight loss and metabolic syndrome in the microbiome era
Eur. Rev. Med. Pharmacol. Sci., 22 (21) (2018), pp. 7588-7605
View Record in ScopusGoogle Scholar[261]
C.S. Johnston, C.S. Day, P.D. Swan
Postprandial thermogenesis is increased 100% on a high-protein, low-fat diet versus a high-carbohydrate, low-fat diet in healthy, young women
J. Am. Coll. Nutr., 21 (2002), pp. 55-61 View PDF
CrossRefView Record in ScopusGoogle Scholar[262]
B.V. Howard, J.E. Manson, M.L. Stefanick, S.A. Beresford, G. Frank, B. Jones, R.J. Rodabough, L. Snetselaar, C. Thomson, L. Tinker, M. Vitolins, R. Prentice
Low-fat dietary pattern and weight change over 7 years: the Women’s Health Initiative Dietary Modification Trial
JAMA, 295 (1) (2006), pp. 39-49 View PDF
CrossRefView Record in ScopusGoogle Scholar[263]
B.V. Howard, L. Van Horn, J. Hsia, J.E. Manson, M.L. Stefanick, S. Wassertheil-Smoller, L.H. Kuller, A.Z. LaCroix, R.D. Langer, N.L. Lasser, C.E. Lewis, M.C. Limacher, K.L. Margolis, W.J. Mysiw, J.K. Ockene, L.M. Parker, M.G. Perri, L. Phillips, R.L. Prentice, J. Robbins, J.E. Rossouw, G.E. Sarto, I.J. Schatz, L.G. Snetselaar, V.J. Stevens, L.F. Tinker, M. Trevisan, M.Z. Vitolins, G.L. Anderson, A.R. Assaf, T. Bassford, S.A. Beresford, H.R. Black, R.L. Brunner, R.G. Brzyski, B. Caan, R.T. Chlebowski, M. Gass, I. Granek, P. Greenland, J. Hays, D. Heber, G. Heiss, S.L. Hendrix, F.A. Hubbell, K.C. Johnson, J.M. Kotchen
Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial
JAMA, 295 (6) (2006), pp. 655-666 View PDF
CrossRefView Record in ScopusGoogle Scholar[264]C.E. Ramsden, D. Zamora, S. Majchrzak-Hong, e. al., Re-evaluation of the traditional diet-heart hypothesis: analysis of recovered data from Minnesota Coronary Experiment (1968-73), BMJ (Clinical research ed.) 353 (2016) i1246.
Google Scholar[265]I.D. Frantz, E.A. Dawson, P.L. Ashman, e. al., Test of effect of lipid lowering by diet on cardiovascular risk. The Minnesota Coronary Survey. , Arteriosclerosis. 9 (1989) 129-135.
M.I. Goran, K. Dumke, S.G. Bouret, B. Kayser, R.W. Walker, B. Blumberg
The obesogenic effect of high fructose exposure during early development. Nature reviews
Endocrinology, 9 (8) (2013), pp. 494-500 View PDF
CrossRefView Record in ScopusGoogle Scholar[267]T. Temelkova-Kurktschiev, G. Siegert, S. Bergmann, e. al., Subclinical inflammation is strongly related to insulin resistance but not to impaired insulin secretion in a high risk population for diabetes, Metabolism 51(6) (2002) 743–749.
Google Scholar[268]F. de Vegt, J.M. Dekker, H.G. Ruhé, e. al., Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study, Diabetologia 42(8) (1999) 926–931.
K. Foster-Powell, J. Brand-Miller
International tables of glycemic index
Am. J. Clin. Nutr., 62 (4) (1995), pp. 871S-890S View PDF
M. Slabber, H.C. Barnard, J.M. Kuyl, A. Dannhauser, R. Schall
Effects of a low-insulin-response, energy-restricted diet on weight loss and plasma insulin concentrations in hyperinsulinemic obese females
Am. J. Clin. Nutr., 60 (1) (1994), pp. 48-53 View PDF
CrossRefView Record in ScopusGoogle Scholar[271]
D.S. Ludwig, F.B. Hu, L. Tappy, J. Brand-Miller
Dietary carbohydrates: role of quality and quantity in chronic disease
BMJ (Clinical research ed.), 361 (2018), p. k2340 View PDF
CrossRefView Record in ScopusGoogle Scholar[272]
H.S. Lee, J. Lee
Effects of combined exercise and low carbohydrate ketogenic diet interventions on waist circumference and triglycerides in overweight and obese individuals: a systematic review and meta-analysis
Int. J. Environ. Res. Public Health, 18 (2) (2021)
F. Magkos, M.F. Hjorth, A. Astrup
Diet and exercise in the prevention and treatment of type 2 diabetes mellitus
Nat. Rev. Endocrinol., 16 (10) (2020), pp. 545-555 View PDF
CrossRefView Record in ScopusGoogle Scholar[274]
H. Li, Y. Dun, W. Zhang, B. You, Y. Liu, S. Fu, L. Qiu, J. Cheng, J.W. Ripley-Gonzalez, S. Liu
Exercise improves lipid droplet metabolism disorder through activation of AMPK-mediated lipophagy in NAFLD
Life Sci., 273 (2021), Article 119314
ArticleDownload PDFView Record in ScopusGoogle Scholar[275]
A. Thorp, J.G. Stine
Exercise as medicine: the impact of exercise training on nonalcoholic fatty liver disease
Curr. Hepatol. Rep., 19 (4) (2020), pp. 402-411 View PDF
CrossRefView Record in ScopusGoogle Scholar[276]
J.Y. Kim, J.Y. Jeon
Role of exercise on insulin sensitivity and beta-cell function: is exercise sufficient for the prevention of youth-onset type 2 diabetes?
Ann. Pediatric Endocrinol. Metabol., 25 (4) (2020), pp. 208-216
View Record in ScopusGoogle Scholar[277]
T.M. Barber, I. Kyrou, H.S. Randeva, M.O. Weickert
Mechanisms of insulin resistance at the crossroad of obesity with associated metabolic abnormalities and cognitive dysfunction
Int. J. Mol. Sci., 22 (2) (2021)
M. Imierska, A. Kurianiuk, A. Błachnio-Zabielska
The influence of physical activity on the bioactive lipids metabolism in obesity-induced muscle insulin resistance
Biomolecules, 10 (12) (2020)
Y. Sun, S. Ding
ER-mitochondria contacts and insulin resistance modulation through exercise intervention
Int. J. Mol. Sci., 21 (24) (2020)
A.M. Gonzalez-Gil, L. Elizondo-Montemayor
The role of exercise in the interplay between myokines, hepatokines, osteokines, adipokines, and modulation of inflammation for energy substrate redistribution and fat mass loss: a review
Nutrients, 12 (6) (2020)
J.C. Rosa-Neto, L.S. Silveira
Endurance exercise mitigates immunometabolic adipose tissue disturbances in cancer and obesity
Int. J. Mol. Sci., 21 (24) (2020)
N. Soltani, S.M. Marandi, M. Kazemi, N. Esmaeil
The exercise training modulatory effects on the obesity-induced immunometabolic dysfunctions
Diabetes Metabol. Syndrome Obesity: Targets Therapy, 13 (2020), pp. 785-810 View PDF
CrossRefView Record in ScopusGoogle Scholar[283]
C. Laurens, A. Bergouignan, C. Moro
Exercise-released myokines in the control of energy metabolism
Front. Physiol., 11 (2020), p. 91
View Record in ScopusGoogle Scholar[284]
Z. Fan, M. Xu
Exercise and Organ cross talk
Adv, Exp, Med, Biol,, 1228 (2020), pp. 63-76 View PDF
CrossRefView Record in ScopusGoogle Scholar[285]
E. Trovato, V. Di Felice, R. Barone
Extracellular vesicles: delivery vehicles of myokines
Front. Physiol., 10 (2019), p. 522
View Record in ScopusGoogle Scholar[286]
I.J. Vechetti, T. Valentino, C.B. Mobley, J.J. McCarthy
The role of extracellular vesicles in skeletal muscle and systematic adaptation to exercise
J. Physiol., 599 (3) (2021), pp. 845-861 View PDF
CrossRefView Record in ScopusGoogle Scholar[287]A.C. Improta Caria, C.K.V. Nonaka, C.S. Pereira, M.B.P. Soares, S.G. Macambira, B.S.F. Souza, Exercise Training-Induced Changes in MicroRNAs: Beneficial Regulatory Effects in Hypertension, Type 2 Diabetes, and Obesity, Int. J. Mol. Sci. 19(11) (2018).
N. Ehtesham, S. Shahrbanian, M. Valadiathar, S.J. Mowla
Modulations of obesity-related microRNAs after exercise intervention: a systematic review and bioinformatics analysis
Mol. Biol. Rep. (2021)
J.E. Harris, L.A. Baer, K.I. Stanford
Maternal exercise improves the metabolic health of adult offspring
Trends Endocrinol. Metabol.: TEM, 29 (3) (2018), pp. 164-177
ArticleDownload PDFView Record in ScopusGoogle Scholar[290]
J. Zheng, L.Y. Zhou, X.H. Xiao
Maternal exercise and its beneficial effects on glucose metabolism in offspring
Chin Med. J. (Engl), 133 (7) (2020), pp. 863-867 View PDF
CrossRefView Record in ScopusGoogle Scholar[291]
S.F. McCarthy, H. Islam, T.J. Hazell
The emerging role of lactate as a mediator of exercise-induced appetite suppression
Am. J. Physiol. Endocrinol. Metabol., 319 (4) (2020), pp. E814-E819 View PDF
CrossRefView Record in ScopusGoogle Scholar[292]
R.L. Atkinson
Viruses as an etiology of obesity
Mayo Clin Proc, 82 (10) (2007), pp. 1192-1198
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[293]
M.J. Lyons, I.M. Faust, R.B. Hemmes, D.R. Buskirk, J. Hirsch, J.B. Zabriskie
A virally induced obesity syndrome in mice
Science, 216 (4541) (1982), pp. 82-85 View PDF
CrossRefView Record in ScopusGoogle Scholar[294]
J.K. Carter, C.L. Ow, R.E. Smith
Rous-associated virus type 7 induces a syndrome in chickens characterized by stunting and obesity
Infect. Immun., 39 (1) (1983), pp. 410-422 View PDF
CrossRefView Record in ScopusGoogle Scholar[295]R.L. Atkinson, N.V. Dhurandhar, D.B. Allison, R.L. Bowen, B.A. Israel, J.B. Albu, A.S. Augustus, Human adenovirus-36 is associated with increased body weight and paradoxical reduction of serum lipids, International journal of obesity (2005) 29(3) (2005) 281-6.
Q. Shang, H. Wang, Y. Song, L. Wei, C. Lavebratt, F. Zhang, H. Gu
Serological data analyses show that adenovirus 36 infection is associated with obesity: a meta-analysis involving 5739 subjects
Obesity (Silver Spring), 22 (3) (2014), pp. 895-900 View PDF
CrossRefView Record in ScopusGoogle Scholar[297]
E. Ponterio, L. Gnessi
Adenovirus 36 and obesity: an overview
Viruses, 7 (7) (2015), pp. 3719-3740 View PDF
CrossRefView Record in ScopusGoogle Scholar[298]S.D. Vangipuram, M. Yu, J. Tian, K.L. Stanhope, M. Pasarica, P.J. Havel, A.R. Heydari, N.V. Dhurandhar, Adipogenic human adenovirus-36 reduces leptin expression and secretion and increases glucose uptake by fat cells, International journal of obesity (2005) 31(1) (2007) 87-96.
Google Scholar[299]J. Sapunar, L. Fonseca, V. Molina, E. Ortiz, M.I. Barra, C. Reimer, M. Charles, C. Schneider, M. Ortiz, R. Brito, V. Manríquez, M. Pavez, A. Cerda, Adenovirus 36 seropositivity is related to obesity risk, glycemic control, and leptin levels in Chilean subjects, International journal of obesity (2005) 44(1) (2020) 159-166.
D.J. Fazakerley, J.R. Krycer, A.L. Kearney, S.L. Hocking, D.E. James
Muscle and adipose tissue insulin resistance: malady without mechanism?
J. Lipid Res., 60 (10) (2019), pp. 1720-1732
ArticleDownload PDFCrossRefView Record in ScopusGoogle Scholar[301]
D. Samocha-Bonet, V.D. Dixit, C.R. Kahn, R.L. Leibel, X. Lin, M. Nieuwdorp, K.H. Pietiläinen, R. Rabasa-Lhoret, M. Roden, P.E. Scherer, S. Klein, E. Ravussin
Metabolically healthy and unhealthy obese–the 2013 Stock Conference report
Obes Rev., 15 (9) (2014), pp. 697-708 View PDF
CrossRefView Record in ScopusGoogle Scholar[302]
T. Kitamura, C.R. Kahn, D. Accili
Insulin receptor knockout mice
Annu. Rev. Physiol., 65 (2003), pp. 313-332
View Record in ScopusGoogle Scholar[303]
M. Matsumoto, S. Han, T. Kitamura, D. Accili
Dual role of transcription factor FoxO1 in controlling hepatic insulin sensitivity and lipid metabolism
J. Clin. Invest., 116 (9) (2006), pp. 2464-2472
View Record in ScopusGoogle Scholar[304]
M. Naïmi, N. Gautier, C. Chaussade, A.M. Valverde, D. Accili, E. Van Obberghen
Nuclear forkhead box O1 controls and integrates key signaling pathways in hepatocytes
Endocrinology, 148 (5) (2007), pp. 2424-2434 View PDF
CrossRefView Record in ScopusGoogle Scholar[305]
G.F. Lewis, K.D. Uffelman, L.W. Szeto, G. Steiner
Effects of acute hyperinsulinemia on VLDL triglyceride and VLDL apoB production in normal weight and obese individuals
Diabetes, 42 (6) (1993), pp. 833-842 View PDF
CrossRefView Record in ScopusGoogle Scholar[306]
S. Fu, S.M. Watkins, G.S. Hotamisligil
The role of endoplasmic reticulum in hepatic lipid homeostasis and stress signaling
Cell Metab, 15 (5) (2012), pp. 623-634
ArticleDownload PDFView Record in ScopusGoogle Scholar[307]
A.L. Birkenfeld, G.I. Shulman
Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes
Hepatology, 59 (2) (2014), pp. 713-723 View PDF
CrossRefView Record in ScopusGoogle Scholar[308]
J. Sripetchwandee, N. Chattipakorn, S.C. Chattipakorn
Links between obesity-induced brain insulin resistance, brain mitochondrial dysfunction, and dementia
Front. Endocrinol. (Lausanne), 9 (2018), p. 496
View Record in ScopusGoogle Scholar[309]
M. Valdearcos, J.D. Douglass, M.M. Robblee, M.D. Dorfman, D.R. Stifler, M.L. Bennett, I. Gerritse, R. Fasnacht, B.A. Barres, J.P. Thaler, S.K. Koliwad
Microglial inflammatory signaling orchestrates the hypothalamic immune response to dietary excess and mediates obesity susceptibility
Cell Metab., 26 (1) (2017), pp. 185-197.e3
ArticleDownload PDFView Record in ScopusGoogle Scholar[310]
G.F. Lewis, A. Carpentier, K. Adeli, A. Giacca
Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes
Endocr. Rev., 23 (2) (2002), pp. 201-229
View Record in ScopusGoogle Scholar[311]S. Lobo, D.A. Bernlohr, Fatty acid transport in adipocytes and the development of insulin resistance, Novartis Found Symp 286 (2007) 113-21; discussion 121-6, 162-3, 196-203.
B.R. Thompson, S. Lobo, D.A. Bernlohr
Fatty acid flux in adipocytes: the in’s and out’s of fat cell lipid trafficking
Mol. Cell Endocrinol., 318 (1–2) (2010), pp. 24-33
ArticleDownload PDFView Record in ScopusGoogle Scholar[313]
P. Zhao, K.I. Wong, X. Sun, S.M. Reilly, M. Uhm, Z. Liao, Y. Skorobogatko, A.R. Saltiel
TBK1 at the crossroads of inflammation and energy homeostasis in adipose tissue
Cell, 172 (4) (2018), pp. 731-743.e12
ArticleDownload PDFView Record in ScopusGoogle Scholar[314]
A.A. Bremer, S. Devaraj, A. Afify, I. Jialal
Adipose tissue dysregulation in patients with metabolic syndrome
J. Clin. Endocrinol. Metabol., 96 (11) (2011), pp. E1782-E1788 View PDF
CrossRefView Record in ScopusGoogle Scholar[315]
S.E. Shoelson, J. Lee, A.B. Goldfine
Inflammation and insulin resistance
J. Clin. Invest., 116 (7) (2006), pp. 1793-1801 View PDF
CrossRefView Record in ScopusGoogle Scholar[316]
H. Xu, G.T. Barnes, Q. Yang, G. Tan, D. Yang, C.J. Chou, J. Sole, A. Nichols, J.S. Ross, L.A. Tartaglia, H. Chen
Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance
J. Clin. Invest., 112 (12) (2003), pp. 1821-1830
View Record in ScopusGoogle Scholar[317]
A.R. Saltiel, J.M. Olefsky
Inflammatory mechanisms linking obesity and metabolic disease
J. Clin. Invest., 127 (1) (2017), pp. 1-4
View Record in ScopusGoogle Scholar[318]
G. Cildir, S.C. Akincilar, V. Tergaonkar
Chronic adipose tissue inflammation: all immune cells on the stage
Trends Mol. Med., 19 (8) (2013), pp. 487-500
ArticleDownload PDFView Record in ScopusGoogle Scholar[319]
R. Kolb, F.S. Sutterwala, W. Zhang
Obesity and cancer: inflammation bridges the two
Curr. Opin. Pharmacol., 29 (2016), pp. 77-89
ArticleDownload PDFView Record in ScopusGoogle Scholar[320]
C.M. Steppan, E.J. Brown, C.M. Wright, S. Bhat, R.R. Banerjee, C.Y. Dai, G.H. Enders, D.G. Silberg, X. Wen, G.D. Wu, M.A. Lazar
A family of tissue-specific resistin-like molecules
PNAS, 98 (2) (2001), pp. 502-506
View Record in ScopusGoogle Scholar[321]
A. Bansal, J. Henao-Mejia, R.A. Simmons
Immune system: an emerging player in mediating effects of endocrine disruptors on metabolic health
Endocrinology, 159 (1) (2018), pp. 32-45 View PDF
CrossRefView Record in ScopusGoogle Scholar[322]
C. Crewe, Y.A. An, P.E. Scherer
The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis
J Clin Invest, 127 (1) (2017), pp. 74-82
View Record in ScopusGoogle Scholar[323]
S.M. Reilly, A.R. Saltiel
Adapting to obesity with adipose tissue inflammation
Nat. Rev. Endocrinol., 13 (11) (2017), pp. 633-643 View PDF
CrossRefView Record in ScopusGoogle Scholar[324]
L. Russo, C.N. Lumeng
Properties and functions of adipose tissue macrophages in obesity
Immunology, 155 (4) (2018), pp. 407-417 View PDF
CrossRefView Record in ScopusGoogle Scholar[325]
Y. Li, K. Yun, R. Mu
A review on the biology and properties of adipose tissue macrophages involved in adipose tissue physiological and pathophysiological processes
Lipids Health Dis., 19 (1) (2020), p. 164
ArticleDownload PDFGoogle Scholar[326]
O. Osborn, J.M. Olefsky
The cellular and signaling networks linking the immune system and metabolism in disease
Nat. Med., 18 (3) (2012), pp. 363-374, 10.1038/nm.2627 View PDF
View Record in ScopusGoogle Scholar[327]
N. Ouchi, J.L. Parker, J.J. Lugus, K. Walsh
Adipokines in inflammation and metabolic disease
Nat. Rev. Immunol., 11 (2) (2011), pp. 85-97, 10.1038/nri2921
Epub 2011 Jan 21 View PDF
View Record in ScopusGoogle Scholar[328]
H. Sell, C. Habich, J. Eckel
Adaptive immunity in obesity and insulin resistance
Nat. Rev. Endocrinol., 8 (12) (2012), pp. 709-716, 10.1038/nrendo.2012.114
Epub 2012 Jul 31 View PDF
View Record in ScopusGoogle Scholar[329]
J.R. Brestoff, D. Artis
Immune regulation of metabolic homeostasis in health and disease
Cell, 161 (1) (2015), pp. 146-160, 10.1016/j.cell.2015.02.022
ArticleDownload PDFView Record in ScopusGoogle Scholar[330]
M. Itoh, T. Suganami, R. Hachiya, Y. Ogawa
Adipose tissue remodeling as homeostatic inflammation
Int. J. Inflam., 2011 (2011), Article 720926
View Record in ScopusGoogle Scholar[331]
J.O. Hill
Understanding and addressing the epidemic of obesity: an energy balance perspective
Endocr. Rev., 27 (7) (2006), pp. 750-761 View PDF
CrossRefView Record in ScopusGoogle Scholar[332]
R. Sarwar, N. Pierce, S. Koppe
Obesity and nonalcoholic fatty liver disease: current perspectives
Diabet. Metabol. Syndrome Obesity: Targets Therapy, 11 (2018), pp. 533-542 View PDF
CrossRefView Record in ScopusGoogle Scholar[333]
A. Hruby, F.B. Hu
The epidemiology of obesity: a big picture
PharmacoEconomics, 33 (7) (2015), pp. 673-689 View PDF
CrossRefView Record in ScopusGoogle Scholar[334]
J. Durack, S.V. Lynch
The gut microbiome: relationships with disease and opportunities for therapy
J. Exp. Med., 216 (1) (2019), pp. 20-40 View PDF
CrossRefView Record in ScopusGoogle Scholar[335]
A.B. Shreiner, J.Y. Kao, V.B. Young
The gut microbiome in health and in disease
Curr. Opin. Gastroenterol., 31 (1) (2015), pp. 69-75
View Record in ScopusGoogle Scholar[336]
P.D. Cani
Human gut microbiome: hopes, threats and promises
Gut, 67 (9) (2018), pp. 1716-1725 View PDF
CrossRefView Record in ScopusGoogle Scholar[337]
M. Li, B. van Esch, G.T.M. Wagenaar, J. Garssen, G. Folkerts, P.A.J. Henricks
Pro- and anti-inflammatory effects of short chain fatty acids on immune and endothelial cells
Eur. J. Pharmacol., 831 (2018), pp. 52-59
ArticleDownload PDFCrossRefGoogle Scholar[338]
O. Castaner, A. Goday, Y.M. Park, S.H. Lee, F. Magkos, S.T.E. Shiow, H. Schroder
The gut microbiome profile in obesity: a systematic review
Int. J. Endocrinol., 2018 (2018), p. 4095789
L. Abenavoli, E. Scarpellini, C. Colica, L. Boccuto, B. Salehi, J. Sharifi-Rad, V. Aiello, B. Romano, A. De Lorenzo, A.A. Izzo, R. Capasso
Gut microbiota and obesity: a role for probiotics
Nutrients, 11 (11) (2019), p. 2690 View PDF
CrossRefView Record in ScopusGoogle Scholar[340]
J. Qin, R. Li, J. Raes, M. Arumugam, K.S. Burgdorf, C. Manichanh, T. Nielsen, N. Pons, F. Levenez, T. Yamada, D.R. Mende, J. Li, J. Xu, S. Li, D. Li, J. Cao, B. Wang, H. Liang, H. Zheng, Y. Xie, J. Tap, P. Lepage, M. Bertalan, J.M. Batto, T. Hansen, D. Le Paslier, A. Linneberg, H.B. Nielsen, E. Pelletier, P. Renault, T. Sicheritz-Ponten, K. Turner, H. Zhu, C. Yu, S. Li, M. Jian, Y. Zhou, Y. Li, X. Zhang, S. Li, N. Qin, H. Yang, J. Wang, S. Brunak, J. Dore, F. Guarner, K. Kristiansen, O. Pedersen, J. Parkhill, J. Weissenbach, H.I.T.C. Meta, P. Bork, S.D. Ehrlich, J. Wang
A human gut microbial gene catalogue established by metagenomic sequencing
Nature, 464 (7285) (2010), pp. 59-65 View PDF
R.E. Ley, P.J. Turnbaugh, S. Klein, J.I. Gordon
Microbial ecology: human gut microbes associated with obesity
Nature, 444 (7122) (2006), pp. 1022-1023 View PDF
R. Wang, R. Tang, B. Li, X. Ma, B. Schnabl, H. Tilg
Gut microbiome, liver immunology, and liver diseases
Cell Mol. Immunol., 18 (1) (2021), pp. 4-17 View PDF
CrossRefView Record in ScopusGoogle Scholar[343]
T. Aguilar, G.M. Nava, A.M. Olvera-Ramirez, D. Ronquillo, M. Camacho, G.A. Zavala, M.C. Caamano, K. Acevedo-Whitehouse, J.L. Rosado, O.P. Garcia
Gut bacterial families are associated with body composition and metabolic risk markers in school-aged children in rural Mexico
Childhood obesity (Print), 16 (5) (2020), pp. 358-366 View PDF
CrossRefView Record in ScopusGoogle Scholar[344]
A. Sekikawa, T. Kadowaki, J.D. Curb, R.W. Evans, H. Maegawa, R.D. Abbott, K. Sutton-Tyrrell, T. Okamura, C. Shin, D. Edmundowicz, A. Kadota, J. Choo, A. El-Saed, H. Ueshima, L.H. Kuller, E.j.s.
group, Circulating levels of 8 cytokines and marine n-3 fatty acids and indices of obesity in Japanese, white, and Japanese American middle-aged men
J. Interferon Cytokine Res., 30 (7) (2010), pp. 541-548 View PDF
CrossRefView Record in ScopusGoogle Scholar[345]
J. Henao-Mejia, E. Elinav, C. Jin, L. Hao, W.Z. Mehal, T. Strowig, C.A. Thaiss, A.L. Kau, S.C. Eisenbarth, M.J. Jurczak, J.P. Camporez, G.I. Shulman, J.I. Gordon, H.M. Hoffman, R.A. Flavell
Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity
Nature, 482 (7384) (2012), pp. 179-185 View PDF
CrossRefView Record in ScopusGoogle Scholar[346]
V.K. Ridaura, J.J. Faith, F.E. Rey, J. Cheng, A.E. Duncan, A.L. Kau, N.W. Griffin, V. Lombard, B. Henrissat, J.R. Bain, M.J. Muehlbauer, O. Ilkayeva, C.F. Semenkovich, K. Funai, D.K. Hayashi, B.J. Lyle, M.C. Martini, L.K. Ursell, J.C. Clemente, W. Van Treuren, W.A. Walters, R. Knight, C.B. Newgard, A.C. Heath, J.I. Gordon
Gut microbiota from twins discordant for obesity modulate metabolism in mice
Science, 341 (6150) (2013), p. 1241214
View Record in ScopusGoogle Scholar[347]
A. Agus, J. Planchais, H. Sokol
Gut microbiota regulation of tryptophan metabolism in health and disease
Cell Host. Microbe., 23 (6) (2018), pp. 716-724
ArticleDownload PDFView Record in ScopusGoogle Scholar[348]
L. Laurans, N. Venteclef, Y. Haddad, M. Chajadine, F. Alzaid, S. Metghalchi, B. Sovran, R.G.P. Denis, J. Dairou, M. Cardellini, J.M. Moreno-Navarrete, M. Straub, S. Jegou, C. McQuitty, T. Viel, B. Esposito, B. Tavitian, J. Callebert, S.H. Luquet, M. Federici, J.M. Fernandez-Real, R. Burcelin, J.M. Launay, A. Tedgui, Z. Mallat, H. Sokol, S. Taleb
Genetic deficiency of indoleamine 2,3-dioxygenase promotes gut microbiota-mediated metabolic health
Nat. Med., 24 (8) (2018), pp. 1113-1120 View PDF
CrossRefView Record in ScopusGoogle Scholar[349]
S. Sanna, N.R. van Zuydam, A. Mahajan, A. Kurilshikov, A. Vich Vila, U. Vosa, Z. Mujagic, A.A.M. Masclee, D. Jonkers, M. Oosting, L.A.B. Joosten, M.G. Netea, L. Franke, A. Zhernakova, J. Fu, C. Wijmenga, M.I. McCarthy
Causal relationships among the gut microbiome, short-chain fatty acids and metabolic diseases
Nat Genet, 51 (4) (2019), pp. 600-605 View PDF
CrossRefView Record in ScopusGoogle Scholar[350]
H. Xiao, S. Kang
The Role of the Gut Microbiome in Energy Balance With a Focus on the Gut-Adipose Tissue Axis
Front Genet, 11 (2020), p. 297
View Record in ScopusGoogle Scholar[351]
H. Tilg, N. Zmora, T.E. Adolph, E. Elinav
The intestinal microbiota fuelling metabolic inflammation
Nat. Rev. Immunol., 20 (1) (2020), pp. 40-54 View PDF
CrossRefView Record in ScopusGoogle Scholar[352]
A.T. Virtue, S.J. McCright, J.M. Wright, M.T. Jimenez, W.K. Mowel, J.J. Kotzin, L. Joannas, M.G. Basavappa, S.P. Spencer, M.L. Clark, S.H. Eisennagel, A. Williams, M. Levy, S. Manne, S.E. Henrickson, E.J. Wherry, C.A. Thaiss, E. Elinav, J. Henao-Mejia
The gut microbiota regulates white adipose tissue inflammation and obesity via a family of microRNAs
Sci Transl Med, 11 (496) (2019)
J. Boursier, O. Mueller, M. Barret, M. Machado, L. Fizanne, F. Araujo-Perez, C.D. Guy, P.C. Seed, J.F. Rawls, L.A. David, G. Hunault, F. Oberti, P. Cales, A.M. Diehl
The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota
Hepatology, 63 (3) (2016), pp. 764-775 View PDF
CrossRefView Record in ScopusGoogle Scholar[354]
L. Fandriks
Roles of the gut in the metabolic syndrome: an overview
J. Int. Med., 281 (4) (2017), pp. 319-336 View PDF
CrossRefView Record in ScopusGoogle Scholar[355]
A. Kohsaka, J. Bass
A sense of time: how molecular clocks organize metabolism
Trends Endocrinol. Metabol.: TEM, 18 (1) (2007), pp. 4-11
ArticleDownload PDFView Record in ScopusGoogle Scholar[356]
J.J. Gooley
Circadian regulation of lipid metabolism
Proc. Nutr. Soc., 75 (4) (2016), pp. 440-450
View Record in ScopusGoogle Scholar[357]
A. Mayeuf-Louchart, M. Zecchin, B. Staels, H. Duez
Circadian control of metabolism and pathological consequences of clock perturbations
Biochimie, 143 (2017), pp. 42-50
ArticleDownload PDFView Record in ScopusGoogle Scholar[358]
Y. Serin, N. Acar Tek
Effect of Circadian Rhythm on Metabolic Processes and the Regulation of Energy Balance
Ann. Nutr. Metab., 74 (4) (2019), pp. 322-330 View PDF
CrossRefView Record in ScopusGoogle Scholar[359]
D. Guan, M.A. Lazar
Interconnections between circadian clocks and metabolism
J. Clin. Invest., 131 (15) (2021)
S.G. Parkar, A. Kalsbeek, J.F. Cheeseman
Potential role for the gut microbiota in modulating host circadian rhythms and metabolic health
Microorganisms, 7 (2) (2019)
A. Mukherji, S.M. Bailey, B. Staels, T.F. Baumert
The circadian clock and liver function in health and disease
J. Hepatol., 71 (1) (2019), pp. 200-211
ArticleDownload PDFView Record in ScopusGoogle Scholar[362]
X. Pan, S. Mota, B. Zhang
Circadian clock regulation on lipid metabolism and metabolic diseases
Adv. Exp. Med. Biol., 1276 (2020), pp. 53-66 View PDF
CrossRefView Record in ScopusGoogle Scholar[363]
A.R. Saran, S. Dave, A. Zarrinpar
Circadian rhythms in the pathogenesis and treatment of fatty liver disease
Gastroenterology, 158 (7) (2020), pp. 1948-1966.e1
ArticleDownload PDFView Record in ScopusGoogle Scholar[364]C. Andriessen, P. Schrauwen, J. Hoeks, The importance of 24-h metabolism in obesity-related metabolic disorders: opportunities for timed interventions, International journal of obesity (2005) 45(3) (2021) 479-490.
D.J. Barker
The fetal and infant origins of adult disease
BMJ (Clinical research ed.), 301 (6761) (1990), p. 1111 View PDF
CrossRefView Record in ScopusGoogle Scholar[366]
D.J. Barker
The origins of the developmental origins theory
J. Intern. Med, 261 (5) (2007), pp. 412-417 View PDF
CrossRefView Record in ScopusGoogle Scholar[367]
E. Oken, M.W. Gillman
Fetal origins of obesity
Obes. Res., 11 (4) (2003), pp. 496-506 View PDF
CrossRefView Record in ScopusGoogle Scholar[368]
P.D. Taylor, L. Poston
Developmental programming of obesity in mammals
Exp Physiol, 92 (2) (2007), pp. 287-298 View PDF
CrossRefView Record in ScopusGoogle Scholar[369]
C.N. Hales, D.J. Barker, P.M. Clark, L.J. Cox, C. Fall, C. Osmond, P.D. Winter
Fetal and infant growth and impaired glucose tolerance at age 64
BMJ (Clinical research ed.), 303 (6809) (1991), pp. 1019-1022 View PDF
CrossRefView Record in ScopusGoogle Scholar[370]
G.C. Curhan, W.C. Willett, E.B. Rimm, D. Spiegelman, A.L. Ascherio, M.J. Stampfer
Birth weight and adult hypertension, diabetes mellitus, and obesity in US men
Circulation, 94 (12) (1996), pp. 3246-3250
View Record in ScopusGoogle Scholar[371]
G.C. Curhan, G.M. Chertow, W.C. Willett, D. Spiegelman, G.A. Colditz, J.E. Manson, F.E. Speizer, M.J. Stampfer
Birth weight and adult hypertension and obesity in women
Circulation, 94 (6) (1996), pp. 1310-1315
View Record in ScopusGoogle Scholar[372]
I. Rogers, E.-B.S. Group
The influence of birthweight and intrauterine environment on adiposity and fat distribution in later life
Int. J. Obesity Related Metabolic Disorders : J. Int. Assoc. Study of Obesity, 27 (7) (2003), pp. 755-777
K.K. Ong, M.L. Ahmed, P.M. Emmett, M.A. Preece, D.B. Dunger
Association between postnatal catch-up growth and obesity in childhood: prospective cohort study
BMJ (Clinical research ed.), 320 (2000)
L. Ibáñez, K. Ong, D.B. Dunger, F. de Zegher
Early development of adiposity and insulin resistance after catch-up weight gain in small-for-gestational-age children
J. Clin. Endocrinol. Metabol., 91 (6) (2006), pp. 2153-2158 View PDF
CrossRefView Record in ScopusGoogle Scholar[375]
T.I. Halldorsson, D. Rytter, L.S. Haug, B.H. Bech, I. Danielsen, G. Becher, T.B. Henriksen, S.F. Olsen
Prenatal exposure to perfluorooctanoate and risk of overweight at 20 years of age: a prospective cohort study
Environ. Health Perspect. (2012)
J.M. Braun, A. Chen, M.E. Romano, A.M. Calafat, G.M. Webster, K. Yolton, B.P. Lanphear
Prenatal perfluoroalkyl substance exposure and child adiposity at 8 years of age: The HOME study
Obesity (Silver Spring), 24 (1) (2016), pp. 231-237 View PDF
CrossRefView Record in ScopusGoogle Scholar[377]
M. Vrijheid, S. Fossati, L. Maitre, S. Marquez, T. Roumeliotaki, L. Agier, S. Andrusaityte, S. Cadiou, M. Casas, M. de Castro, A. Dedele, D. Donaire-Gonzalez, R. Grazuleviciene, L.S. Haug, R. McEachan, H.M. Meltzer, E. Papadopouplou, O. Robinson, A.K. Sakhi, V. Siroux, J. Sunyer, P.E. Schwarze, I. Tamayo-Uria, J. Urquiza, M. Vafeiadi, A. Valentin, C. Warembourg, J. Wright, M.J. Nieuwenhuijsen, C. Thomsen, X. Basagana, R. Slama, L. Chatzi
Early-life environmental exposures and childhood obesity: an exposome-wide approach
Environ. Health Perspect., 128 (6) (2020), p. 67009
Google Scholar[378]E. Oken, E.B. Levitan, M.W. Gillman, Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis, International journal of obesity (2005) 32(2) (2008) 201-10.
C.M. Boney, A. Verma, R. Tucker, B.R. Vohr
Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus
Pediatrics, 115 (3) (2005), pp. e290-e296 View PDF
CrossRefView Record in ScopusGoogle Scholar[380]
T.J. Roseboom, J.H. van der Meulen, A.C. Ravelli, C. Osmond, D.J. Barker, O.P. Bleker
Effects of prenatal exposure to the Dutch famine on adult disease in later life: an overview
Mol Cell Endocrinol, 185 (1–2) (2001), pp. 93-98
ArticleDownload PDFView Record in ScopusGoogle Scholar[381]
C.S. Yajnik, H.G. Lubree, S.S. Rege, S.S. Naik, J.A. Deshpande, S.S. Deshpande, C.V. Joglekar, J.S. Yudkin
Adiposity and hyperinsulinemia in Indians are present at birth
J. Clin. Endocrinol. Metabol., 87 (12) (2002), pp. 5575-5580
View Record in ScopusGoogle Scholar[382]
N.J. Arends, V.H. Boonstra, H.J. Duivenvoorden, P.L. Hofman, W.S. Cutfield, A.C. Hokken-Koelega
Reduced insulin sensitivity and the presence of cardiovascular risk factors in short prepubertal children born small for gestational age (SGA)
Clin. Endocrinol., 62 (1) (2005), pp. 44-50 View PDF
CrossRefView Record in ScopusGoogle Scholar[383]
C.J. Petry, S.E. Ozanne, C.L. Wang, C.N. Hales
Effects of early protein restriction and adult obesity on rat pancreatic hormone content and glucose tolerance
Horm Metab Res, 32 (6) (2000), pp. 233-239 View PDF
CrossRefView Record in ScopusGoogle Scholar[384]
R.A. Simmons, L.J. Templeton, S.J. Gertz
Intrauterine growth retardation leads to the development of type 2 diabetes in the rat
Diabetes, 50 (10) (2001), pp. 2279-2286 View PDF
CrossRefView Record in ScopusGoogle Scholar[385]
S.G. Bouret, R.B. Simerly
Minireview: Leptin and development of hypothalamic feeding circuits
Endocrinology, 145 (2004), pp. 2621-2626
View Record in ScopusGoogle Scholar[386]
S. Pinto, A.G. Roseberry, H. Liu, S. Diano, M. Shanabrough, X. Cai, J.M. Friedman, T.L. Horvath
Rapid rewiring of arcuate nucleus feeding circuits by leptin
Science, 304 (5667) (2004), pp. 110-115
View Record in ScopusGoogle Scholar[387]
M.H. Vickers, P.D. Gluckman, A.H. Coveny, P.L. Hofman, W.S. Cutfield, A. Gertler, B.H. Breier, M. Harris
Neonatal leptin treatment reverses developmental programming
Endocrinology, 146 (10) (2005), pp. 4211-4216 View PDF
CrossRefView Record in ScopusGoogle Scholar[388]
A.P. Starling, J.T. Brinton, D.H. Glueck, A.L. Shapiro, C.S. Harrod, A.M. Lynch, A.M. Siega-Riz, D. Dabelea
Associations of maternal BMI and gestational weight gain with neonatal adiposity in the Healthy Start study
Am. J. Clin. Nutr., 101 (2) (2015), pp. 302-309 View PDF
CrossRefView Record in ScopusGoogle Scholar[389]
P.M. Catalano, N.M. Drago, S.B. Amini
Maternal carbohydrate metabolism and its relationship to fetal growth and body composition
Am. J. Obstet. Gynecol., 172 (5) (1995), pp. 1464-1470
ArticleDownload PDFView Record in ScopusGoogle Scholar[390]
R.C. Whitaker, W.H. Dietz
Role of the prenatal environment in the development of obesity
J. Pediat., 132 (5) (1998), pp. 768-776
ArticleDownload PDFView Record in ScopusGoogle Scholar[391]
D.A. Lawlor, G.D. Smith, M. O’Callaghan, R. Alati, A.A. Mamun, G.M. Williams, J.M. Najman
Epidemiologic evidence for the fetal overnutrition hypothesis: findings from the mater-university study of pregnancy and its outcomes
Am. J. Epidemiol., 165 (4) (2007), pp. 418-424
View Record in ScopusGoogle Scholar[392]
B.L. Silverman, L. Landsberg, B.E. Metzger
Fetal hyperinsulinism in offspring of diabetic mothers. Association with the subsequent development of childhood obesity
Ann N Y Acad Sci, 699 (1993), pp. 36-45 View PDF
CrossRefView Record in ScopusGoogle Scholar[393]
B.L. Silverman, T.A. Rizzo, N.H. Cho, B.E. Metzger
Long-term effects of the intrauterine environment
The Northwestern University Diabetes in Pregnancy Center, Diabetes Care, 21 (Suppl 2) (1998), pp. B142-B149
View Record in ScopusGoogle Scholar[394]
J.G. Kral, S. Biron, S. Simard, F.S. Hould, S. Lebel, S. Marceau, P. Marceau
Large maternal weight loss from obesity surgery prevents transmission of obesity to children who were followed for 2 to 18 years
Pediatrics, 118 (6) (2006), pp. e1644-e1649 View PDF
CrossRefView Record in ScopusGoogle Scholar[395]
S. Pinney, R. Simmons
Metabolic programming, epigenetics, and gestational diabetes mellitus
Curr. Diab.Rep., 12 (1) (2012), pp. 67-74 View PDF
CrossRefView Record in ScopusGoogle Scholar[396]
K.E. Boyle, Z.W. Patinkin, A.L.B. Shapiro, C. Bader, L. Vanderlinden, K. Kechris, R.C. Janssen, R.J. Ford, B.K. Smith, G.R. Steinberg, E.J. Davidson, I.V. Yang, D. Dabelea, J.E. Friedman
Maternal obesity alters fatty acid oxidation AMPK activity, and associated DNA methylation in mesenchymal stem cells from human infants
Mol. Metabol., 6 (11) (2017), pp. 1503-1516
ArticleDownload PDFView Record in ScopusGoogle Scholar[397]
M.J. Heerwagen, M.R. Miller, L.A. Barbour, J.E. Friedman
Maternal obesity and fetal metabolic programming: a fertile epigenetic soil
Am. J. Physiol. Regul. Integr. Comp. Physiol., 299 (3) (2010), pp. R711-R722 View PDF
CrossRefView Record in ScopusGoogle Scholar[398]
C. Allard, V. Desgagne, J. Patenaude, M. Lacroix, L. Guillemette, M.C. Battista, M. Doyon, J. Menard, J.L. Ardilouze, P. Perron, L. Bouchard, M.F. Hivert
Mendelian randomization supports causality between maternal hyperglycemia and epigenetic regulation of leptin gene in newborns
Epigenetics, 10 (4) (2015), pp. 342-351 View PDF
J.J. Heindel, F.S. vom Saal
Role of nutrition and environmental endocrine disrupting chemicals during the perinatal period on the aetiology of obesity
Mol. Cell Endocrinol., 304 (1–2) (2009), pp. 90-96
ArticleDownload PDFView Record in ScopusGoogle Scholar[400]
R. Barouki, E. Melén, Z. Herceg, J. Beckers, J. Chen, M. Karagas, A. Puga, Y. Xia, L. Chadwick, W. Yan, K. Audouze, R. Slama, J. Heindel, P. Grandjean, T. Kawamoto, K. Nohara
Epigenetics as a mechanism linking developmental exposures to long-term toxicity
Environ. Int., 114 (2018), pp. 77-86
ArticleDownload PDFView Record in ScopusGoogle Scholar[401]
P.L. Hofman, F. Regan, W.E. Jackson, C. Jefferies, D.B. Knight, E.M. Robinson, W.S. Cutfield
Premature birth and later insulin resistance
New Engl. J. Med., 351 (21) (2004), pp. 2179-2186
View Record in ScopusGoogle Scholar[402]
N.P. French, R. Hagan, S.F. Evans, M. Godfrey, J.P. Newnham
Repeated antenatal corticosteroids: size at birth and subsequent development
Am. J. Obstet. Gynecol., 180 (1 Pt 1) (1999), pp. 114-121
ArticleDownload PDFView Record in ScopusGoogle Scholar[403]
S.L. Bloom, J.S. Sheffield, D.D. McIntire, K.J. Leveno
Antenatal dexamethasone and decreased birth weight
Obstet. Gynecol., 97 (4) (2001), pp. 485-490
ArticleDownload PDFView Record in ScopusGoogle Scholar[404]S. Entringer, S. Wüst, R. Kumsta, I.M. Layes, E.L. Nelson, D.H. Hellhammer, P.D. Wadhwa, Prenatal psychosocial stress exposure is associated with insulin resistance in young adults, Am J Obstet Gynecol 199(5) (2008) 498.e1-7.
K.L. Tamashiro, C.E. Terrillion, J. Hyun, J.I. Koenig, T.H. Moran
Prenatal stress or high-fat diet increases susceptibility to diet-induced obesity in rat offspring
Diabetes, 58 (5) (2009), pp. 1116-1125 View PDF
CrossRefView Record in ScopusGoogle Scholar[406]
T.F. Oberlander, J. Weinberg, M. Papsdorf, R. Grunau, S. Misri, A.M. Devlin
Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses
Epigenetics, 3 (2) (2008), pp. 97-106 View PDF
CrossRefView Record in ScopusGoogle Scholar[407]
M.F. Dallman, N.C. Pecoraro, S.E. la Fleur
Chronic stress and comfort foods: self-medication and abdominal obesity
Brain Behav. Immun., 19 (4) (2005), pp. 275-280
ArticleDownload PDFView Record in ScopusGoogle Scholar[408]
M.F. Dallman, N. Pecoraro, S.F. Akana, S.E. La Fleur, F. Gomez, H. Houshyar, M.E. Bell, S. Bhatnagar, K.D. Laugero, S. Manalo
Chronic stress and obesity: a new view of “comfort food”
PNAS, 100 (20) (2003), pp. 11696-11701
View Record in ScopusGoogle Scholar
Tradução livre, parcial, de Luiz Jacques Saldanha, maio de 2022.


